Explore Our Blog


According to a recent Deloitte study, 76% of American companies outsource their IT functions. What drives this trend? Does outsourcing truly win the in-house vs outsourcing development battle? In this article, we will explore both strategies, evaluate their advantages and disadvantages, and help you choose the approach that best suits your project.

What Is In-House and Outsourcing Software Development?
In-house development refers to the process in which a company independently creates its digital products. In this case, only the internal team is involved in development, without hiring external specialists.
Do you think this approach is ideal because all IT functions will be handled by a reliable development team that you assemble yourself? In some ways, you’re right. However, it also comes with significant responsibility and high costs. After all, you will need to hire and manage developers, designers, product and project managers, and other personnel. But we will discuss the pros and cons of this strategy in more detail later.
Outsourcing software development implies hiring an external team or individual remote specialists to work on a software solution. Depending on the budget size, required technology stack, and other project specifics, you can choose between nearshoring, offshoring, and onshoring. What do these terms mean?
Offshoring refers to delegating processes to a distant country, often on another continent. This is considered the most cost-effective outsourcing option, as service rates vary significantly across countries. However, such price differences do not always affect the quality of the final product.
Take a look at these impressive figures: In Switzerland, developers earn around $100,000 per year, whereas in Norway, Australia, and several other countries, this amount is nearly half as much. Does this mean that specialists in those regions are less qualified? Hardly.

Nearshoring—outsourcing to a neighboring country. Preferably one that borders yours or is at least located on the same continent. The goal is usually the same—to save on IT services.
Onshoring—hiring external specialists from your own country. What is the point? It’s simple. Even within the same state, the cost of creating an identical digital solution can vary significantly.
As an example, take a look at the salary range in major USA cities (data provided by Indeed):
- Columbus, OH – $142,605 per year
- Bellevue, WA – $137,206 per year
- San Jose, CA – $120,751 per year
- San Diego, CA – $118,932 per year
- Houston, TX – $98,751 per year
So, we have figured out the definitions of in-house and outsourced software development and also discussed the types of the latter. What are the key differences between these strategies?
In-House vs Outsourcing: Key Differences
In-house vs outsourcing development is a choice that many teams face. The fact is that there are several fundamental differences between these approaches. They should be taken into account when organizing the development process in a company.

This comparison highlights the strengths and weaknesses of both approaches to software development. However, to make these differences even clearer, let's take a closer look at the pros and cons of outsourcing and in-house development.
Outsourcing Software Development: Pros and Cons
Let’s start by looking at outsourcing software development – the pros and cons of this approach allow the global outsourcing market to grow at an impressive rate. This suggests that the cons of this approach are not so significant, right?
If in 2024 it was valued at $611.8 billion, it is projected to grow to $1,345.5 billion in the next 10 years.

Outsourced Development Pros
Teams that opt for outsourcing digital solution development can expect the following benefits:
1. Cost Savings.
We’ve already mentioned that companies can save by outsourcing to regions with cheaper labor.
However, that’s not all. Toptal has created a calculator to estimate the actual costs of hiring in-house developers and remote specialists. According to the calculations, even with the same hourly rate, outsourcing will cost the company 1.5 times less:

This is explained by additional expenses for office rent, employee training, providing necessary infrastructure, and so on.
2. Access to the global talent pool.
Finding a developer with the necessary skills can be challenging, especially in regions where the number of specialists is not very large.
Take a look at how the number of IT specialists differs in various countries:

Access to the global talent pool allows you to use the latest technologies that may not be widely available in your region.
3. Flexibility and scalability.
According to Indeed, the hiring process can take anywhere from a week to a month or more! Therefore, if you anticipate the need to expand or reduce your team, it is wiser to consider outsourcing.
It also makes more sense to consider a remote candidate for short-term projects if there is no further collaboration planned after the project ends.
4. Accelerating Time to Market.
Outsourcing allows you to reduce the time spent on recruiting and hiring specialists. Additionally, there is no need for training and onboarding the development team, which, as you’d agree, is also a lengthy process.
Moreover, you can engage several teams to work on the project. They will work on different aspects of the application simultaneously, bringing its release closer. An additional benefit is the ability to work around the clock due to time zone differences.
5. Optimization of company operations.
Outsourcing IT functions will allow you to focus on other activities, such as marketing, customer service, implementing financial strategies, and more.
Furthermore, outsourcing makes sense even if you have an in-house development team. Engaging external specialists will reduce the load on your team and allow you to implement innovative technologies that your developers may not be proficient in.
Outsourced Development Cons
Along with the benefits for a company, turning to IT outsourcing can lead to certain challenges:
1. Communication problems.
This issue is especially relevant with offshoring, when specialists are located in different time zones. Just imagine: you need to urgently address an issue, but it's outside your team's working hours. This can seriously affect the efficiency of development.
Another possible barrier to productive collaboration is different languages and cultural differences. Wouldn't it be difficult to understand your counterpart if their vocabulary is unfamiliar to you, or if they adhere to values and traditions that differ from yours?
2. Quality control challenges.
When an in-house team is working on a software product, they are clearly aware of the standards they need to follow. This enables them to create solutions that meet the needs of the audience and business expectations.
In the case of outsourced development, there is a risk of discrepancies in quality standards between internal and external teams, especially when communication gaps exist.
The result is an unsatisfactory final product, which may lead to another outsourcing drawback—as we'll discuss next.
3. Hidden costs.
If the final product quality is lacking, you’ll have to hire other specialists to fix defects. However, this problem can be avoided by working only with trusted providers.
Still, there is the risk of additional costs for managing remote specialists and the possibility of project expansion due to control issues.
4. Data and intellectual property (IP) security.
Collaborating with third parties on development involves sharing confidential information about your business and clients.
Again, only work with reliable partners to ensure they won’t misuse your data or share it with unauthorized individuals.
We’ve discussed the pros and cons of outsourcing software development. How does the situation look with the advantages and disadvantages of creating an in-house team?
In-House Development: Pros and Cons
Despite the growing popularity of outsourcing, many companies still prefer to develop software in-house. This approach also has its own pros and cons.
In-house Development Pros
Developing software internally offers the following advantages:
1. Full control over the development process.
The decision to hire an in-house team is a step towards complete control over the development process.
You can select the optimal tech stack, implement methodologies that you deem suitable, and track every stage of the SDLC and its duration.
2. Intellectual property security.
According to ABI Research, U.S. companies lose between $180 billion and $540 billion annually due to intellectual property theft.
In-house development minimizes the likelihood of this issue, as the company will be the sole owner, and there is no need to share data with third parties.
3. Improved communication on the project.
Teams working in a shared workspace experience fewer communication challenges. They are not hindered by cultural and language differences or time zone discrepancies.
This, in turn, helps avoid several problems. According to recent statistics, poor communication methods can lead to a number of losses for a company. Among these, 68% of work time is wasted, 42% of employees face stress and burnout, and 12% of customers leave for competitors:

4. Team engagement and a deep understanding of business nuances.
An internal development team is likely to be better informed about the company's values, culture, and target audience. This enables them to create a tailored solution that aligns with the client’s vision.
Additionally, in-house developers are more invested in the success of the project, as they are part of the business.
In-house Development Cons
If you are an advocate of in-house development, be prepared for some challenges along with the benefits. Here are a few of them:
1. High costs.
With outsourcing, the company only spends money on the developer’s rate. The situation is completely different with an in-house team.
We present a list of expenses to consider:
- hiring costs;
- total salary of the team;
- provision of necessary infrastructure;
- training fees for technologies;
- bonuses and benefits;
- software license purchases;
- overhead costs.
Overall, the difference between in-house vs outsourcing development can amount to hundreds of thousands of dollars. And as you can see, it is not in favor of the in-house team.
2. Limited resources.
In-house specialists may have limited experience and knowledge in specific areas needed for the project. There are two solutions to this issue: employee training, which again incurs additional costs and time, or opting for familiar technologies that are unlikely to yield the desired results.
Moreover, the lack of resources may become noticeable when scaling the project significantly. Hiring an in-house specialist is a lengthy and complicated process.
3. Hiring issues and employee turnover.
According to Statista's analytics, in 2023, 54% of organizations experienced a shortage of tech talent. And this is not the peak — two years ago, this figure was at a record-high 70%.

However, even if you manage to hire the best talents, don’t rush to celebrate your victory. You still need to retain them. And here’s where the real challenge begins. To attract a developer to work specifically for your company, you will need to offer a high salary (higher than your competitors), social benefits, bonuses, etc. In other words, you will be committing yourself to unforeseen expenses. Whether this is justified is up to you to decide.
So, we’ve thoroughly discussed the advantages and disadvantages of in-house development and outsourcing. Now, it’s time to determine which strategy is best suited for you.
In-House vs Outsourcing: How to Make the Right Choice?
In-house vs outsourcing software development—which one should you choose for your company’s success? Here are the types of projects optimal for each of these strategies:
For in-house development:
- Long-term projects. If a project requires constant development, support, and close collaboration, it makes sense to build an internal team. This is especially relevant for complex systems that are continuously evolving and require in-depth knowledge of their architecture.
- Projects involving confidential data. If you are dealing with confidential data, in-house development can guarantee its complete security. This is facilitated by better control over work processes and the absence of the need to share data with third parties.
However, as an alternative, you can turn to a reliable outsourcing provider who guarantees the security of confidential data on par with an in-house team.
- Projects that are critical for the business. These are projects that involve creating products that must fully reflect the vision, culture, and strategy of the company. If you are not sure that you can achieve this with external developers, it is better to opt for an in-house team.
For outsourced development:
- Projects with a limited budget. Outsourcing allows savings on developer salaries and related expenses.
- Short-term projects. If the team is only required to create a product without further updates and support, hiring in-house specialists is not advisable.
- Projects where quick time-to-market is a priority. Time savings on hiring and adaptation, the ability for round-the-clock work, and involving multiple teams contribute to faster releases.
- Projects with changing resource needs. Here, the ability of remote teams to scale quickly is key.
- Innovative projects. Access to a global talent pool enables the use of cutting-edge technologies that may not be well-developed in your region.
Thus, if you are looking to save costs, use an innovative tech stack, and outpace competitors, outsourced development will be the best choice for your company.
Darly Solutions—Your Reliable Partner in Outsourced Software Development
The Darly Solutions team is ready to be your guide in the world of creating high-quality digital solutions. We provide comprehensive services, including web and mobile development, UI/UX design, MVP development, QA and testing, and much more.
By outsourcing your project to us, you can be confident in our full immersion in your product vision, data and intellectual property security, and guaranteed adherence to project deadlines.
Contact a Darly Solutions manager, calculate the estimated costs, and start your journey to digitalization today!


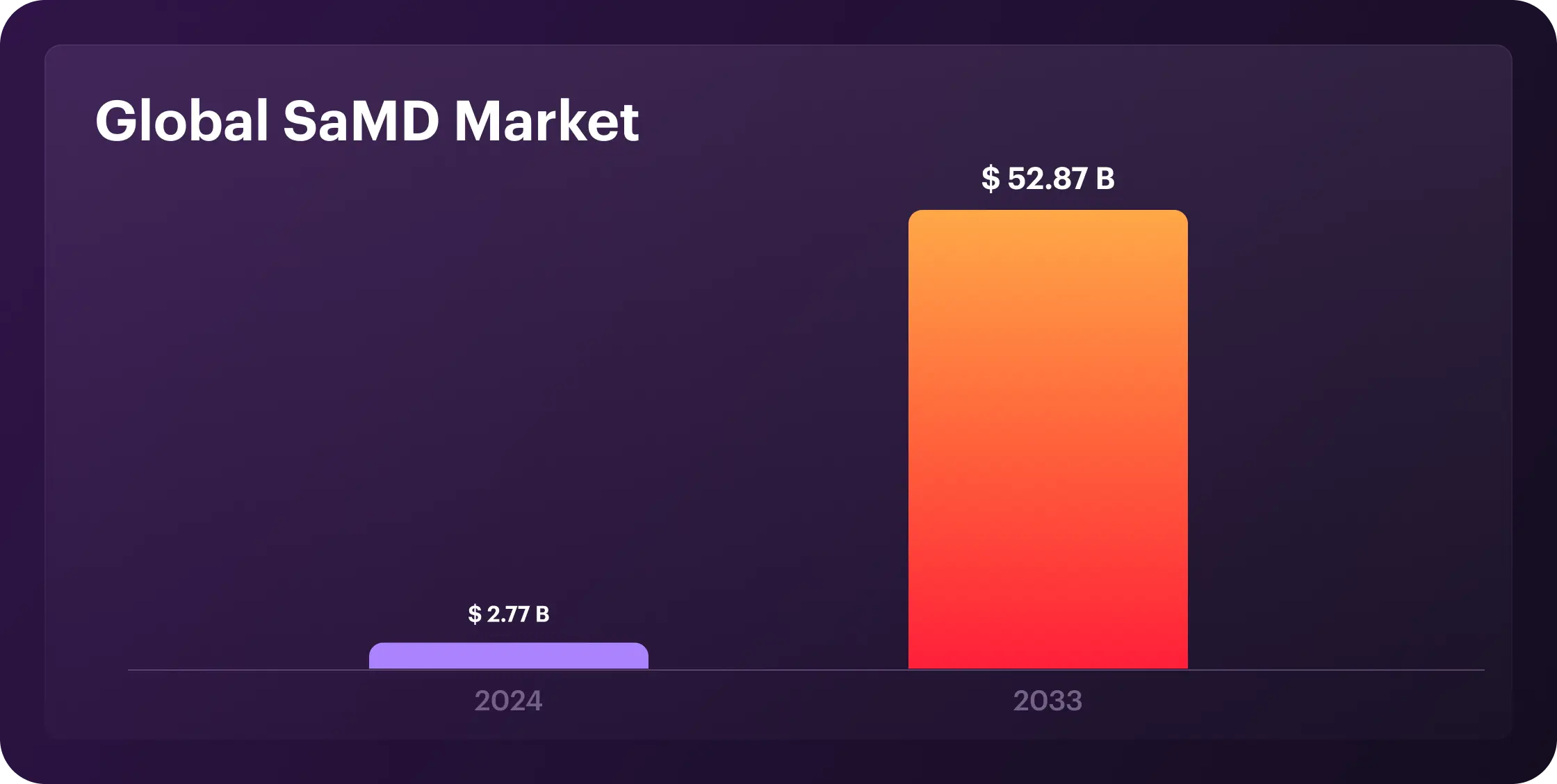
Medical device software now drives the core of digital health. AI powers diagnostics, IoT connects patients to providers, and real-time data shifts care from reactive to predictive. According to recent statistics, the global SaMD market is projected to grow from $2.77 billion in 2024 to $52.87 billion by 2033 at a compound annual growth rate (CAGR) of 38.4%. The U.S. advances rapidly with FDA pathways designed for speed, while Europe maintains a GDPR-compliant digital health infrastructure, holding a 30% global market share.
Nevertheless, the future is bright for SaMD; it has benefits and challenges. Let's dive into the meaning of medical device software development, including the steps and types.
What Is Medical Device Software Development?
Medical device software development refers to designing, creating, testing, and maintaining software that is integral to the functionality of medical devices or operates as a standalone medical device. This software must meet strict regulations for safety and accuracy, including those from the FDA, MDR, and ISO 13485.
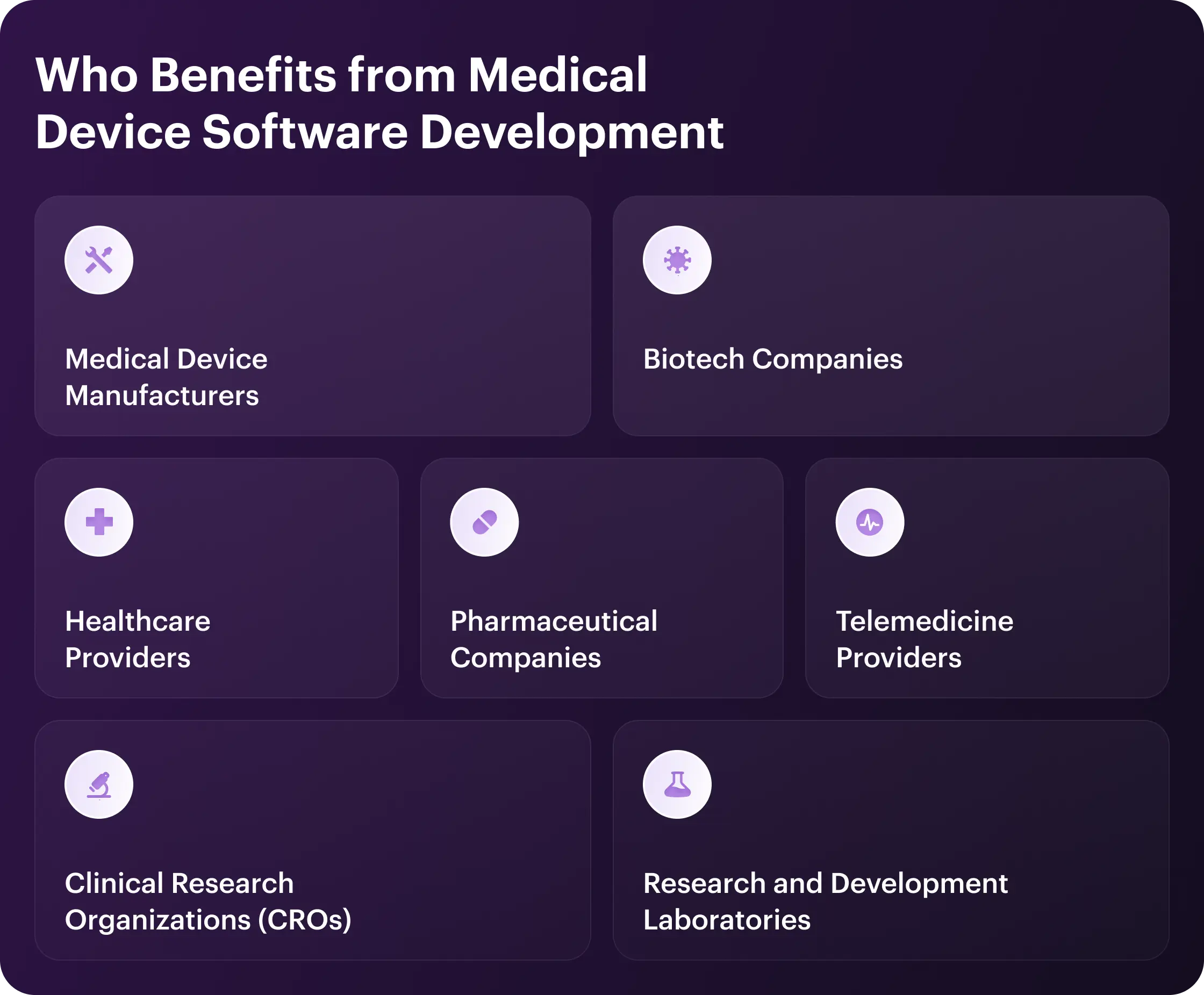
Who Benefits from Medical Device Software Development
Demand for medical device software spans many sectors. Let's explore the industries leading the way.
Healthcare Providers
Real-time patient data helps providers make sharper decisions and diagnoses. Automation reduces manual errors and allows staff to focus on care. AI and IoT add efficiency and enable remote, personalized treatment. This delivers faster, safer care while cutting costs.
Medical Device Manufacturers
Medical device manufacturers use software to automate quality control and ensure compliance with regulations. Real-time monitoring reduces errors and helps make proactive adjustments. Scalable updates future-proof devices, while ERP systems improve supply chains, reduce costs, and accelerate time-to-market.
Pharmaceutical Companies
Pharma firms cut trial costs via wearables, automate drug production with digital batch records, and monetize AI-powered SaMD apps that improve adherence. Real-time monitoring speeds up approvals, while AI-driven data tailors therapies and unlocks revenue from digital treatments and SaaS models, sharpening efficiency and market edge.
Telemedicine Providers
Telemedicine thrives in video conferencing and remote monitoring, particularly in underserved areas. Yet, it needs specialized software to connect with medical devices for remote diagnosis, monitoring, and treatment. Modern medical device software improves access to care, diagnostic accuracy, patient engagement, and chronic disease management while also helping reduce hospital readmissions.
Biotech Companies
Biotech companies use medical device software to process complex biological data, speed up drug discovery, and perform diagnostics. Custom tools automate tasks while ensuring compliance with FDA and HIPAA regulations, reducing risk. The result? This tech drives innovation, cuts costs, and accelerates the development of market-ready biotech products.
Clinical Research Organizations (CROs)
CROs gain efficiency and accuracy through automated data handling in device trials. Better data management and real-time monitoring improve trial quality and speed. This leads to faster market entry, reduced costs, and ensured regulatory compliance.
Research and Development Laboratories
Medical device software transforms R&D labs. Thus, teams automate tasks, use AI for sharper data analysis, and lock in compliance from day one. As a result, labs hit faster diagnostics, therapies, and disease control breakthroughs without slowdowns.
Advantages of Software Development for Medical Devices
Software is the new heartbeat of healthcare, making devices smarter, faster, and more efficient. Better outcomes and lower costs are just the beginning. Discover the full positive impact below.
Increased diagnostic accuracy
Medical device software improves diagnostic precision through advanced data analysis techniques. Algorithms detect subtle patterns humans might miss, especially in imaging and laboratory results. Machine learning models continually refine their accuracy by analyzing millions of patient cases, significantly reducing error rates.
In practice, whole-slide imaging in digital pathology achieves a diagnostic concordance of 96.5%, matching that of traditional light microscopy. AI models like GPT-4 show pooled diagnostic accuracy of 52.1%, on par with non-expert physicians but still below experts by 15.8%
Process automation
Automation eliminates repetitive tasks, reduces errors, and allows medical staff to focus on patients. The software handles everything from scheduling to medication management, reducing costs while boosting efficiency. Hospitals report significant time savings and happier staff after implementing automated systems.
Real-time patient monitoring
Connected devices track vital signs without constant staff presence. The software alerts doctors when readings breach safe thresholds for immediate intervention. This capability saves lives in ICUs and helps patients with unpredictable chronic conditions.
Integration with medical systems
Medical software integrates with hospital databases, electronic health records, and laboratory systems. This eliminates data silos and ensures all providers see complete patient information. System interoperability reduces duplicate data entry and lowers the risk of transcription errors.
For instance, integrated medical software reduces duplicate data entry by 30% and transcription errors by over 50%. Hospitals with connected EHR and lab systems report a 25% boost in care coordination and faster clinical decisions.
Regulatory compliance
Built-in audit trails, access controls, and encryption protect patient data while meeting legal medical device software standards. These safeguards prevent costly violations and data breaches that damage trust and finances.
Flexibility and scalability
Medical software adapts to changing needs through modular design and cloud deployment. Solutions scale from single clinics to hospital networks without performance loss. Providers start with core functions and expand as requirements evolve.
Remote access and telemedicine
Telemedicine breaks geographical barriers to healthcare delivery. Remote monitoring enables home recovery while maintaining professional oversight. These systems maintain care continuity during emergencies when facilities reach capacity.
Cost reduction
Software-driven automation delivers significant savings through improved efficiency. Predictive maintenance prevents equipment failures and reduces downtime. Digital transformation reduces administrative overhead, with hospitals reporting a 30% decrease in operational costs.
Improved user experience
Intuitive interfaces cut training needs and boost adoption among medical staff. Human-centered medical device software design makes complex technology accessible to everyone. Patient apps improve treatment adherence with simple instructions and timely reminders.
Support for analytics and AI
Analytics transform medical data into actionable insights for treatment. AI identifies high-risk patients before acute episodes occur. Machine learning models continually improve with new clinical data, keeping recommendations updated with medical advances.

Key Aspects to Consider in Medical Device Software Development
Medical device software revolutionizes healthcare, but building it is no walk in the park. From regulations and compatibility to testing and ongoing maintenance, the stakes are high, and the margin for error is zero in medical device software development. Here's what matters most and saves lives.
Meeting Regulatory Standards
Regulatory compliance is non-negotiable. Developers must navigate a maze of standards from bodies like the FDA or EMA, which classify software based on risk and dictate the approval process. Whether it's a 510(k) or a PMA, getting them wrong can result in costly delays or outright rejection. Stay updated, plan for compliance from day one, and document everything—regulators love paperwork.
Ensuring Data Security and Privacy
Medical software handles sensitive patient data, which makes security a top priority. Encryption, secure authentication, and regular audits are must-haves to protect against breaches. HIPAA and GDPR aren't just guidelines—they're the law. One misstep can lead to hefty fines and a PR nightmare, so lock it down.
Designing for Usability and User-Centered Experience
If your software design for medical devices isn't user-friendly, it's a liability. Engage with doctors, nurses, or patients early and often to design interfaces that reduce errors and fit seamlessly into their workflows. Accessibility isn't optional—it's essential. A confusing UI can lead to misdiagnoses or delays, so make it intuitive and easy to use.
Ensuring Compatibility with Healthcare Systems
The software never lives in a vacuum. It must comply with EHRs, LIS, or PACS, using standards like HL7 or DICOM. Since interoperability isn't just a buzzword—it's how data flows smoothly in healthcare—build with flexibility in mind. Systems change, and your software should keep up.
Implementing Effective Risk Mitigation
Risk management is baked into medical software development. Use frameworks like ISO 14971 to identify hazards, assess risks, and implement controls to manage them. Plus, tools like FMEA help catch issues before they become disasters. In this field, an ounce of prevention is worth a pound of cure.
Thorough Testing and Quality Validation
From unit tests to clinical validation, every layer counts. Rigorous validation, covering unit, integration, system, and user acceptance testing, helps catch defects early. Include performance, security, and interoperability checks. Pay attention to documenting everything: regulators will demand proof.
Ongoing Maintenance and Software Enhancement
Launch day is just the beginning. Bugs, security patches, and new features require constant attention. Set up a robust post-market surveillance plan to catch issues early. Your software should evolve with healthcare, not fall behind.
Types of Medical Device Software
Based on hardware and regulatory integration, medical device software falls into two primary categories:
Embedded Software for Medical Systems (EMSSW)
This type of software is an integral part of medical devices, such as pacemakers, infusion pumps, and imaging machines. Embedded systems control device functions, ensuring they operate safely and effectively. It is not standalone software like desktop or mobile apps, and it cannot function without the hardware of the medical device.
Examples of Embedded Software for Medical Systems (EMSSW) are:
- Pulse oximeters.
- Smart bio-sensors.
- Glucometers.
- Electronic blood pressure sensors.
- Medical imaging devices, such as X-rays, MRIs, and CT scans.
Standalone Software as a Medical Device (SaMD)
Standalone Software as a Medical Device (SaMD) performs a medical function independently of dedicated hardware. Think algorithms spotting heart issues in ECGs or apps managing diabetes. Regulated by the FDA and EU MDR, it operates on phones, laptops, or clouds, slashing costs and supercharging care delivery.
Examples of Standalone Software as a Medical Device (SaMD):
- Patient imaging or scan analysis.
- Remote ECG-monitoring.
- MRI Viewing applications.
Steps in Medical Device Software Development
When lives depend on technology, there's no room for error. Follow the steps of medical device software development grounded in timeless principles: safety, usability, and trust.
Comprehend Regulatory Standards
Compliance encompasses global frameworks such as IEC 62304 (software lifecycle management) and ISO 13485 (quality management), as well as regional mandates, including FDA design controls in the U.S. and MDR/IVDR in the EU. Data privacy laws, such as HIPAA in the U.S. and GDPR in the EU, govern the handling of patient information. Developers must integrate these standards early, ensuring risk management, usability testing, and documentation meet audit requirements. A deep understanding of these rules prevents costly delays and ensures software reliability in clinical settings.
Conduct Market Research and Identify User Needs
Research market trends and competitors to define your software's unique value. To gather user needs, engage stakeholders, such as clinicians, patients, and administrators, through interviews or surveys. Translate these into clear use cases and functional requirements aligned with clinical workflows.
Select an Experienced Development Partner
Choose a development partner with proven expertise in medical device software and IEC 62304 compliance. Ensure they understand relevant regulations, such as FDA or EU MDR, and can support submissions and audits. Verify their technical skills in areas such as embedded systems or AI, and confirm that they follow rigorous testing protocols. Prioritize clear communication and strong project management to meet your timeline and goals.
Development and System Integration
Adopt an iterative development approach, such as Agile, tailored to IEC 62304 to balance flexibility and traceability. Design a modular software architecture for scalability and integration with hardware or external systems, such as EHRs, using standards like HL7 or FHIR. Follow secure coding practices and document code for compliance. Integrate software with hardware or APIs, then conduct thorough verification and validation through unit, integration, and system testing to ensure safety and performance.
Deployment and Ongoing Monitoring
Prepare regulatory submissions, such as a 510(k) for the FDA or a Technical File for EU MDR, to gain market approval. Deploy the software in phases, starting with pilot testing in clinical settings to validate real-world performance, train users to ensure proper operation, and minimize errors. Implement post-market surveillance per ISO 13485 to monitor performance, collect feedback, and address adverse events. Use analytics to track usage and identify issues, such as cybersecurity threats.
Ongoing Support and Maintenance
Provide prompt bug fixes and updates to enhance functionality or security, ensuring compliance with regulations for significant changes. Offer user support through helpdesks or chatbots to resolve issues. Plan periodic upgrades to keep up with new clinical needs and technologies. Prepare for software end-of-life by managing data migration and complying with data retention rules.

How to Select the Best Medical Device Software Development Company for Your Project?
First, clearly define your project goals and requirements. List specific features like AI diagnostics or cloud integration, compliance needs (e.g., FDA, EU MDR), and budget constraints. Identify the target users, such as clinicians or patients, to guide usability expectations. This ensures you communicate precise needs to potential vendors.
Second, research companies with a proven track record in medical device software. Check portfolios for projects like remote monitoring or EHR-integrated tools. Review client feedback on platforms like Clutch or KLAS Research. Confirm their experience with regulatory approvals, such as ISO 13485 or CE marking.
Third, evaluate their regulatory expertise. Ask how they handle standards like HIPAA, IEC 62304, or FDA guidelines. Request examples of compliance documentation or successful submissions. Strong regulatory knowledge prevents delays and costly revisions.
Fourth, assess their technical capabilities. Verify expertise in your required tech stack, such as IoT, HL7/FHIR for interoperability, or secure cloud platforms like AWS. Ensure they can integrate with healthcare systems and support cross-platform development. Technical alignment reduces risks and boosts performance.
Fifth, prioritize cybersecurity expertise. Confirm they follow secure medical device software engineering practices like OWASP's S-SDLC and use encryption and authentication. Ask about their process for regular updates and vulnerability patches. Robust security protects patient data and builds trust.
Sixth, check their focus on user-centric design. Review examples of intuitive, compliant interfaces for medical devices. Ensure they conduct UX research to minimize user errors. A user-friendly design improves adoption and care outcomes.
Seventh, confirm their collaboration and transparency. Look for clear communication, detailed project plans, and methodologies such as Agile or Scrum. Request clarity on pricing, timelines, and milestones. Transparent collaboration aligns the project with your vision.
Eighth, compare costs while prioritizing value. Expect custom medical software to cost between $ 200,000 and $400,000, depending on its complexity. Ensure they offer scalable solutions and ongoing support. Choose a vendor that strikes a balance between quality and budget without compromising on standards.
Finally, shortlist 3-5 companies and request detailed proposals from them. Conduct interviews to assess their approach, certifications, and alignment with your goals. Select the partner with the best mix of expertise, reliability, and transparency. Sign a contract only after reviewing terms and ensuring mutual clarity.
The Future of Medical Device Software Development
Medical device software already stands at the cutting edge of healthcare innovation, driving massive change in how we diagnose and treat patients. Yet, with billions of dollars flowing into health tech and regulatory barriers easing, the future of medical device software development is bright for the coming years.
AI and Machine Learning Integration
AI algorithms are already making waves in the medical device software sector. Predictive analytics and personalized treatments help spot patterns humans miss, delivering faster diagnoses and better outcomes. The tech now works across nearly every medical specialty, and the trends show it won't stop soon, only evolve.
Cybersecurity as Priority
Security doesn't leave the center stage as connected medical devices face sophisticated threats. Manufacturers now build in encryption, strong authentication, and continuous security monitoring from day one. Patient data protection matters as much as clinical functionality.
Edge Computing Implementation
Processing moves to the device itself, shortening wait times for essential procedures. The tech works even when networks fail, and it is a game-changer for implantables and wearables. Edge computing delivers real-time insights exactly when patients need them.
Interoperability Standards
The industry finally tackles its fragmentation problem with standards that work. FHIR and open APIs create true connectivity between previously siloed systems. The seamless data flow means better decisions based on complete patient records.
Sustainability and Scalability
Developers focus on energy-efficient software to extend the battery life of devices. Modular designs allow easy updates without replacing hardware. Cloud integration supports scaling for large patient populations. This reduces costs and environmental impact.
Regulatory Evolution
Regulators are finally catching up to tech innovation with more flexible frameworks. The FDA and international bodies now offer pre-certification pathways and real-world performance monitoring. Companies can innovate faster while still proving their products are safe.
Why Darly Solutions is Your Best Medical Device Software Partner?
No cookie-cutter code here. We're healthcare tech experts who solve real problems. For hospitals, clinics, and MedTech startups, we've delivered over 60 projects that handle messy data, strict compliance, and seamless integration.
Every solution is tailored, whether you're upgrading old systems or launching new ones. Our tech stack is healthcare-tested: secure, compliant, and built to last. Here's how we do it:
Our services cover:
- Custom software development for unique workflows.
- App development that works across devices.
- Cross-platform solutions to reach more patients.
- Automation services to slash admin time.
- UI/UX design that the medical staff actually uses.
- Integration services to connect legacy systems.
We build dashboards that act, not just display. Our scheduling tools cut admin work in half while keeping patients happy. Need e-prescribing or billing that's both secure and fast? We've done it reliably on a large scale.
Need experts who speak healthcare? Whether it's a whole managed IT team or project-specific help, we're here. Outsource your software development to us, and let's build tools that save time, money, and lives.
Conclusion
Medical device software development is more than code—it's about building tools that make healthcare smarter, safer, and faster. With the right partner, you get solutions that boost outcomes, cut costs, and keep you ahead of the curve. Darly Solutions brings deep healthcare expertise, proven results, and a relentless focus on real-world impact. If you're ready to transform your healthcare business, Darly Solutions is the team to trust.


Budgets are tight, tech demands are high, and in-house teams can’t keep up. Outsourcing IT in healthcare is the solution. Why? Speed and savings. Outsourcing slashes time-to-market for critical tech and delivers top-tier talent on demand. In fact, 23.43% of IT outsourcing globally is healthcare-related. Beyond cost-cutting, there are many other advantages.
Healthcare IT Outsourcing Statistics:
- 30-60% cost reduction is achievable due to healthcare.
- 90% of hospitals in the US have outsourced at least 1 IT service.
- 70% of healthcare organizations plan to increase their IT outsourcing budgets in the next three years.
- 85% of healthcare executives report improved efficiency and productivity from IT outsourcing.
- 60% of healthcare providers have outsourced their EHR management.
- 50% of telehealth in the US is managed by outsourced IT services.
And everything seems bright, yet the pros and cons of outsourcing healthcare persist. Now, let’s explore the meaning of healthcare IT outsourcing, the types of healthcare IT outsourcing, the commonly outsourced services, and the ideas of how to choose the best vendor for healthcare IT outsourcing to help you make an informed decision.
What Is IT Outsourcing in Healthcare?
Healthcare IT outsourcing means hiring external tech experts to handle tasks that aren’t core to patient care. As systems become more complex, providers outsource everything: telehealth, cybersecurity, data entry, billing, and transcription. This lets them focus on patients while staying up to date with technology.
Key Benefits of Outsourcing in Healthcare
Some stats to note: Hiring external IT experts speeds up project delivery by 33% compared to in-house teams. Skipping full-time hires saves over $100K per senior developer each year. Cutting internal recruitment slashes operational costs by 28%, freeing up the budget for core healthcare priorities. Nevertheless, the numbers speak for themselves; organizations must balance these pros and cons of outsourcing healthcare services to align strategy with healthcare’s core mission: delivering safe, compliant, and patient-first care.
Cost Reduction
First of all, outsourcing IT cuts costs by reducing in-house teams. It also replaces large hardware investments with pay-as-you-go services, such as cloud storage. This combination makes IT a predictable cost, freeing up funds for clinical needs.
Access to Specialized Expertise
Outsourcing IT gives healthcare providers instant access to expertise in EHRs, AI, cybersecurity, and blockchain, keeping them ahead of the curve in tech. Vendors already have specialized skills (e.g., AI diagnostics) and apply best practices from multiple clients. For example, vendors can apply innovations, such as robotic process automation for billing, that individual providers or internal teams may not be able to develop internally.
Faster Implementation of Technologies
Outsourcing IT allows healthcare providers to implement new solutions, such as cloud EHRs, telehealth, or advanced analytics, much faster than handling them in-house, thanks to vendors’ ready-made tools and specialized staff. This speeds up deployment, avoids overloading internal teams, and enables 24/7 progress across time zones. As a result, clinics and hospitals can quickly adopt the latest technologies and stay competitive without straining their own resources.
Focus on Core Healthcare Services
Clinicians and managers no longer need to fix servers or coding—external tech specialists handle it. This shift helps smaller practices save time; one clinic recovers hours each week by outsourcing scheduling and EHR support. Large hospitals free up their internal IT teams to focus on strategic priorities, such as care coordination, rather than routine maintenance.
Improved Scalability and Flexibility
Healthcare demand shifts quickly, often due to seasonal spikes, epidemics, or service expansions. Outsourced IT offers instant scalability. Vendors scale teams and systems up or down as needed. A hospital adding clinics can immediately extend the vendor’s support and network. Growing practices get more helpdesk or storage without major upfront costs.
Optimizing Patient Services
24/7 IT support minimizes system downtime and service delays. AI and RPA automate tasks like appointment reminders and claims processing, cutting wait times. Expert-built telehealth platforms boost remote monitoring for rural patients. Outsourced revenue cycle management speeds up billing and claims processing, reducing patient financial surprises.

Potential Drawbacks and Risks of Outsourcing IT in Healthcare
Healthcare IT outsourcing brings big wins—but also big risks. Know how to manage the most common ones.
Data Security and Privacy Concerns
Outsourcing IT in healthcare raises privacy risks because sensitive patient data goes to external vendors. Each transfer creates vulnerabilities, especially if a partner’s security is weak. Breaches can expose records, violate HIPAA or GDPR, and erode trust. Providers lose some control over data protection, and inconsistent security practices add to the risk. Organizations must pick partners with strong security credentials to minimize exposure, which requires encryption, multi-factor authentication, regular audits, and strict contracts.
Compliance with Healthcare Regulations
Healthcare IT outsourcing partners must follow strict regulations, such as HIPAA, GDPR, and local laws. Non-compliance brings heavy fines. Cross-border deals add complexity to US hospital outsourcing to the EU, which must meet GDPR, and vice versa. Vendors must sign BAAs and match the provider’s policies since any partner failure is the provider’s liability. Cloud platforms like AWS and Azure are only compliant if they are correctly configured and covered by Business Associate Agreements (BAAs). Always check for certifications (such as ISO 27001, SOC 2, and HITRUST) and demand proof of compliance. Legal review and clear contracts are essential, but global rules can slow down deals.
Communication Barriers
Language differences and technical jargon can cause misunderstandings. Cultural variations in work style (e.g., how strictly deadlines are followed) can further complicate coordination. Time zone gaps can mean that real-time collaboration suffers—a US clinic’s urgent issue may require overnight handling by an offshore team. Tasks can slip or be misinterpreted without regular, structured communication (such as weekly calls and project management tools).
Loss of Control Over Certain Processes
Outsourcing IT in healthcare means losing direct control over critical functions, which can lead to quality and security issues. Without hands-on oversight, providers cannot enforce their quality standards or catch errors, such as misconfigurations or coding bugs, in real-time. For example, an unsupervised IT helpdesk or feature rollout might deviate from security protocols. Overreliance on SLAs leaves providers powerless to address service drops beyond the contractual escalation process. Malicious or underperforming vendors might prioritize other clients or cut corners.
Technical Barriers to Seamless Integration
Outsourced systems must integrate smoothly within existing healthcare IT (in-house EHRs, lab systems, and workflows), which is often more complex. Moreover, integrating new solutions with legacy infrastructure can be challenging, especially if the existing infrastructure is outdated or uses different technology standards. Thus, discrepancies in processes can fragment workflows, such as those caused by different coding standards or software platforms. Testing and validation often take longer when multiple teams are involved. To overcome this, providers need robust integration planning: use APIs, middleware, or interoperability standards (like HL7 FHIR) and involve in-house IT early in the design. Nonetheless, some level of technical friction is almost inevitable, and providers must allocate resources for system integration and ongoing maintenance across vendors.

Commonly Outsourced Services in the Healthcare Industry
Healthcare is outsourcing smarter than ever. From IT support to billing, cybersecurity, and HR, these services help streamline operations, reduce costs, and keep the focus where it belongs—on patients. Read on for the most common services outsourced in the healthcare industry:
IT Infrastructure and Support Services
Many providers outsource their entire IT helpdesk, network management, and cloud services. For instance, hospitals increasingly rely on managed services for server upkeep and cloud platforms. An outsourced team can manage data backups, firewall maintenance, and user support 24/7. It is often more cost-effective than maintaining a large in-house infrastructure team.
Insurance Claims Management
Outsourcing insurance billing and revenue cycle management (RCM), including claims processing, is a common practice. Vendors with healthcare expertise can handle coding, claim submission, denial management, and collections. Using Robotic Process Automation (RPA) in RCM is a growing trend: automated bots can verify insurance coverage or submit claims 24/7. Put simply, vendors execute routine tasks in a fraction of the time by automating transactional and repetitive processes, which directly benefits revenue cycles. And the result? Faster payment turnaround and fewer denials.
HR and Administrative Operations
External firms often handle non-clinical back-office functions, such as payroll, staffing, recruitment, and human resources. Outsourced HR specialists can recruit nurses and technicians, manage benefits enrollment, and ensure compliance with labor laws. This offloads the administrative burden from medical staff.
Medical Documentation and Coding
Accurate medical coding, using ICD, CPT, and HCPCS codes, is crucial for both billing and compliance. Many practices outsource coding to specialized firms or offshore teams. This guarantees access to certified coders and up-to-date knowledge of coding rules. Studies confirm that outsourced coding ensures accuracy, maintains compliance, and reduces claim denials. Plus, faster claim submissions across time zones improve cash flow.
Healthcare Data Analysis
Firms may hire external data experts to sift through EHR data for population health management, predictive modeling, or operational improvements. For example, a health system might employ a vendor to flag readmission risks or optimize staffing. These partners use AI/ML tools to uncover insights from large datasets, providing access to advanced analytics platforms and data scientists without the need for costly in-house teams. Plus, cloud-based analytics (AWS, Azure, GCP) enable complex modeling and dashboards, with specialists handling HIPAA-compliant pipelines.
Patient and Client Support Services
Many patient-facing administrative tasks are outsourced to call centers or virtual assistants. This includes scheduling appointments, pre-visit insurance verification, nurse triage hotlines, and follow-up calls with patients. Modern outsourcing even incorporates AI: healthcare chatbots can answer common questions or provide medication reminders. Thus, a BPO firm or a hospital might route after-hours calls to an offshore nurse advice line, which keeps patients supported 24/7 and reduces the load on busy office staff.

How to Choose the Right IT Outsourcing Partner
Once you’ve defined the pros and cons of IT outsourcing in healthcare, set clear goals and scope—identify required IT functions, establish your budget, and define desired outcomes to guide every decision. Next, assess your internal capabilities and identify any gaps, so you can target partners with the right expertise in healthcare systems, cloud computing, AI, or cybersecurity.
Research vendors’ reputations, review case studies and speak with references to confirm their track record and financial stability. Verify HIPAA and GDPR compliance, encryption standards, multi-factor authentication, and audit practices to safeguard patient data. Evaluate cultural fit, communication style, and time-zone overlap to ensure smooth collaboration. Negotiate a clear contract with detailed SLAs, performance metrics, pricing models, and exit clauses to align expectations and manage risks.
Develop a transition and knowledge transfer plan that covers data migration, team onboarding, and training to minimize disruptions. Finally, set up ongoing governance with regular performance reviews, reporting dashboards, and feedback loops to drive continuous improvement and keep your partnership on track.
The Future of IT Outsourcing in Healthcare
The healthcare IT outsourcing market is set to explode, doubling from $60.6 billion in 2025 to $117.1 billion by 2035. Hospitals and clinics worldwide now outsource EHR management, analytics, cybersecurity, and revenue cycle ops to cut costs and speed up digital transformation. AI and machine learning drive predictive analytics, automate admin work, and secure patient data. Blockchain gains traction for medical records and fraud prevention. RPA bots handle claims, billing, and scheduling, which reduces errors and boosts efficiency.

Cloud adoption is leading in North America and Europe, with providers transitioning to hybrid and multi-cloud setups for increased scalability and flexibility. Outsourcing partners help even small clinics access enterprise-grade cloud and analytics. Demand for telehealth and IoMT platforms has surged since the pandemic, with many providers outsourcing these services.
Cybersecurity is shifting to managed security service providers as threats rise.
Looking ahead, expect more outsourcing of advanced tech like genomics analysis and virtual reality rehab tools. The market’s growth stems from pressure to cut costs, fill IT skill gaps, and comply with stringent data laws like HIPAA and GDPR. From small clinics to major hospitals, the next decade belongs to providers who turn to outsourcing AI, cloud, and automation.
Darly Solutions—Is Your Proven Vendor of Healthcare IT Outsourcing
Darly Solutions offers end-to-end expertise in healthcare IT, covering everything from core application development to comprehensive back-office and support functions. Our expanded service portfolio taps into industry best practices and proven outsourcing models to help you accelerate innovation, enhance security, and control costs—all while keeping your focus on patient care.
Service Portfolio
- Custom Software Development: BPM, CRM, LIMS, and patient management platforms tailored to your workflows.
- App Development: Native mobile and web apps for telemedicine, remote patient monitoring, and on-the-go clinician tools.
- Cross-Platform Development: Framework-agnostic solutions that run seamlessly on iOS, Android, and web browsers.
- Automation Services: AI-driven RPA for appointment reminders, claims adjudication, and revenue cycle tasks.
- UI/UX Design: Patient-centric interfaces and clinician dashboards that boost engagement and usability.
- Integration Services: Middleware and API management for seamless data exchange.
If you need a managed IT team or project-based augmentation, partner with Darly Solutions to outsource your healthcare software development. Contact us today to transform your digital health initiatives with experts you can trust.
Conclusion
Outsourcing IT in healthcare reduces costs, taps expert talent, accelerates innovation, and scales quickly—ideal for both small clinics and large systems. It frees providers to focus on care, roll out tech like cloud EHRs and AI analytics quickly, and boost service quality with faster billing and 24/7 support.
But it’s not risk-free. Data security, regulatory compliance, and quality must stay airtight. Avoid breaches, integration flops, and control loss by locking down clear contracts, vetting partners hard, and keeping communication sharp.
The smart move? Outsource only non-core IT tasks. Keep sensitive or strategic functions in-house. Treat outsourcing as a long-term strategic play, not just a way to cut costs. Get it right, and it can supercharge your digital health game.


Modern medical centers, clinics, and even general hospitals are gradually transforming their internal processes, focusing on the digitalization of document flow and more. The same applies to billing operations, which are increasing over time.

The popularization of digitalization in payment processes is reflected in the growing demand for specialized systems. According to analysts at Straits Research, the medical billing software niche was valued at $15.34 billion in 2024. According to forecasts from the same source, in 2025 the niche will reach $16.96 billion and will continue to grow at a CAGR of 10.5% until 2033, reaching a total value of $37.68 billion.
There are plenty of reasons for such growth:
- Specialized systems significantly accelerate and automate payment operations.
- They make reporting and taxation processes autonomous.
- They guarantee transaction transparency and compliance with industry standards.
That’s why today we’ll dive deep into the core of medical billing software features. From this material, you will learn about the advantages of such systems, as well as their types, features, and the cost of integration. Familiarize yourself with the article before implementing the appropriate software in your medical facility.
Understanding Medical Billing Software
At first glance, it may seem enough to simply use online banking, POS terminals for accepting payments, keep records in spreadsheets, and not bother with the development, deployment, and configuration of Medical Billing Software. However, unsystematized and manual data management, including payment data, can lead to a number of problems. For example:
- Too many manual operations that require time and resources.
- Risk of revenue loss due to human error.
- Difficulty in accounting and generating reports.
Thus, Medical Billing Software not only automates your facility’s financial operations but also reduces risks, helps to systematize payment processes, reporting, and more. And that’s not all.
Importance of Medical Billing Software in Healthcare

According to a study by Bain & Company, about 80% of respondents—including heads of medical centers—plan to gradually increase spending on IT infrastructure components, including Medical Billing Software.
Why is this so important? For example, because of the advantages and medical billing software features that improve the operational capabilities of healthcare facilities. In particular, we are talking about:
- Automation and improved efficiency of payment processes—that is, minimizing the human factor and reducing the risk of calculation errors.
- Improved transaction accuracy, such as automatic calculation of service costs, report generation, and submission to the appropriate authorities.
- Acceleration of processes—fast information exchange with insurance companies, tax authorities, banks, and other related institutions.
- Compliance with industry standards, such as patient data protection policies and regulations like HIPAA in the United States.
- Increased service satisfaction levels—for example, due to faster billing for patients, simplified payment processes, etc.
- Analytical potential—automated reporting allows the company to better understand the capabilities and needs of the center, plan its development, and control financial flows.
And these are far from all the benefits a medical center receives from integrating specialized software. On the contrary, the key advantages lie in the details—and that’s what we’ll focus on next.
Essential Features of Medical Billing Software
Of the 201 healthcare facility executives in the U.S. who participated in the Bain & Company survey, 56% identified software and technologies as one of the top three strategic development priorities. In other words, the focus on modernizing healthcare provider infrastructure is a trend that will continue for quite a long time.

Among the main priorities for implementing modern IT systems, including Medical Billing Software, the following can be noted:
- User-Friendly Interface.
- Automated Claim Processing.
- Insurance Verification.
- Compliance with Healthcare Regulations.
- Patient Management and Scheduling.
- EHR Integration.
- Customizable Reporting and Analytics.f
- Automated Invoicing and Payment Processing.
- Denial Management and Appeals Tracking.
Let’s go through each point in more detail.
User-Friendly Interface
Traditionally, a fairly large number of tools can be used in medical infrastructure to manage finances. These include spreadsheets for calculations and reporting, third-party programs for data exchange, and external platforms like online banking.
Medical Billing Software offers a unified system with an intuitive and logical interface accessible to employees of all age groups and levels of computer literacy. This somewhat simplifies the learning curve and allows for faster processing of all payment operations—or even their automation.
Automated Claim Processing
Under normal conditions, a patient receives a service and pays for it at the facility’s cashier, right? With specialized billing systems, payment for services provided occurs almost instantly through the issuance of claims.
For example, a doctor or assistant selects the type of service, enters its cost (if it is not fixed), and issues the patient an invoice for payment—either in digital form (such as a QR code) or printed. Payment can be made via the built-in payment aggregator, after which the system automatically issues a receipt and registers the transaction.
Insurance Verification
If the patient’s case is covered by their insurance policy, a request for reimbursement of medical expenses can be submitted immediately after the service is provided.
The system automatically checks the patient’s policy number and the possibility of coverage for treatment. This reduces the time needed for payment processing and eliminates risks, such as denial by the insurance company.
Compliance with Healthcare Regulations
Modern systems must comply with industry requirements such as encryption and overall protection of sensitive data, payment algorithms, etc.
Medical Billing Software typically complies with standards like HIPAA, GDPR, and ISO. In particular, it includes security elements that protect EHR-integrated data, EMR records, account details, transaction information, and more.
Patient Management and Scheduling
Advanced Medical Billing Software platforms go far beyond classic solutions and resemble a mix of ERP/CRM systems with additional accounting and financial functionality.
Thus, even processes like staff scheduling, patient management, appointment coordination, and more can be handled from a single interoperable interface. And yes, staff is divided into roles that are granted access only to specific subsystems. Therefore, confidentiality is maximized.
EHR Integration
To simplify patient management, a secure CRM system can be added to the Medical Billing Software. It allows for real-time updates of data from EHRs present in other compatible medical center networks, insurance references, and so on.
This significantly simplifies doctors' access to patients’ medical histories, allergy information, previous prescriptions, etc. Accordingly, especially in emergency cases, the specialist will be able to provide help to clients faster and more efficiently.
Customizable Reporting and Analytics
Not just automation of reporting, but also its personalization. Medical Billing Software can include several templates for the quick preparation and submission of information to regulators.
For example, reports about a patient’s treatment for subsequent submission to the insurance company, or financial reporting for a certain period to the tax authorities.
Automated Invoicing and Payment Processing
Medical Billing Software can issue invoices in both digital and physical formats. Likewise, it can print receipts or any other payment-related documents.
There is also the option to link patients’ financial data for automatic payment of services or to speed up transactions through a system of instant payments with requests sent to the user’s device.
Denial Management and Appeals Tracking
Even in crisis situations, Medical Billing Software can be a useful asset—for example, when the facility does not receive timely payment from the patient, or the patient disputes the issued invoice.
In such cases, it is possible to track payment progress, justify pricing to the relevant authorities, or even split payments to gradually settle outstanding debts.
Ultimately, the key functionality depends on the type of Medical Billing Software required by a particular healthcare facility. Therefore, next, we’ll look at the available implementation options for such solutions.
Types of Medical Billing Software
If briefly, payment software can be divided into several distinct types. Namely:
- Independent Billing Applications.
- Cloud-Based Billing Platforms.
- Integrated Medical Billing Systems.
- Customized Billing Software.
- EHR-Integrated Billing Solutions.

Medical billing software features will vary depending on the type of system chosen. In fact, so will the cost of development, deployment, and maintenance of each variant listed above.
When choosing software of this class, it should be done in such a way that its functionality and capabilities align as closely as possible with the needs of the facility, and its cost is compensated by the center’s income. Therefore, we offer a more detailed overview of each of the software subtypes and medical billing features.
Independent Billing Applications
Separate solutions used directly for transaction processing, invoicing, and revenue tracking. Typically, they do not integrate with medical systems, so they have poorer compatibility with data.
This type of software can be used in private clinics where the number of patients and staff is quite limited, as well as the profitability, and consequently, the requirements for reporting.
Cloud-Based Billing Platforms
This type of software can offer a better experience with the financial components of medical centers. Traditionally, these are SaaS solutions that are personalized for the needs of specific clinics. Such products can be quite versatile and interoperable.
Typically, solutions of this type have cross-platform performance, so they offer a mobile experience for both the clinic staff and clients. Specifically, this includes the ability for remote management of visit schedules, personal cabinets, one-click payments, and more.
Integrated Medical Billing Systems
Somewhat more complex to implement, but better in potential, these systems can be either SaaS solutions or separate programs that have a modular design and are integrated into the existing digital infrastructure of the clinic.
This type of product is almost universal; however, it offers somewhat worse compatibility with data compared to other platforms and systems. Although, provided that professionals are handling the development and integration, no issues should arise.
Customized Billing Software
Personalized products, often developed in the format of platforms with built-in tools such as ERP, CRM, EDMS, etc. Medical billing software features in such systems are tightly integrated with other components, ensuring instant and secure data exchange.
Note that custom development can offer the most flexible pricing and overall profitability. Yes, it is possible to implement the platform step by step, starting with an MVP, and gradually modernizing the system, scaling it, or transforming it according to the needs of the facility.
EHR-Integrated Billing Solutions
A universal class of systems suitable for facilities that provide a wide range of services to clients. Integration with EHR allows staff to quickly and securely access patient data, as well as store their own information, including treatment course, medical history, contraindications, etc.
This is a rather expensive but the best option for large medical institutions and clinics. Of course, each of the types of systems described can be deployed in any type of hospital. But is it worth it? Let’s also examine this question.
How to Choose the Right Medical Billing Software
It may sound cliché, but your choice should primarily consider the needs of the institution regarding medical billing software features. Here are the factors to pay attention to first:
- Functionality. What and how much needs to be automated, what integrations are necessary, and what financial management capabilities are required.
- Compliance. Primarily with HIPAA, GDPR, ISO standards, or others, if it's critical for the institution.
- Integrations. Specifically with the current infrastructure of the clinic, such as EHR, CRM, and payment aggregators.
- Ease of Use. Intuitiveness and ease of training staff of all age groups.
- Platform Type. Whether it's a local or cloud-based solution, or possibly a hybrid. This will also affect the UX and usage costs.
- Cost. Pricing models for the product, its maintenance, and updates.

If for some reason you are unable to determine what exactly your institution needs, you can always seek help and consultation from the experts at Darly Solutions. In fact, they can also help define an initial estimate for development, integration, deployment, and system maintenance.
Cost of Custom Medical Billing Software Development
Regarding the pricing of products of this type, their range can vary widely. Specifically, the following factors will affect the cost:
- Platform complexity. A basic system may cost around $30,000, while a solution with AI, coding CPT, ICD-10, etc., could be priced starting from $150,000.
- Technologies. The rule is similar—simpler and more accessible systems tend to have a lower product cost.
- Number and complexity of integrations. There is a logical progression as the complexity increases.
- UI/UX design. This depends partly on the chosen technologies but is usually calculated separately.
Security and regulatory compliance. This factor is mostly included in the base development cost, but sometimes it is itemized separately if specific data protection measures are needed.
Development time and team. This is rarely considered as a separate pricing factor, but you will have to pay extra for faster delivery. - Maintenance. Platform upgrades, bug fixes, and routine security patches are usually listed as a separate item.

The cost of creating Medical Billing Software is a dynamic figure, primarily depending on the center's needs and the service provider's pricing. So, if you want to save costs or at least avoid going bankrupt, use Darly Solutions’ help and a step-by-step implementation plan.
Future Trends in Medical Billing Software
This type of software follows all the traditional IT sector trends. Specifically:
- AI and ML for forecasting and automating reporting, analytics, operations, and risk management.
- Integration of blockchain elements for protecting data, transactions, and financial information.
- Development of telemedicine and expansion of IoT potential for use in this field.
- Transition to 100% cloud-based solutions for maximum mobility of medical services.
- Expansion of regulatory requirements aimed at service personalization and patient protection.
The technological horizon is currently quite dynamic, so trends that influence the niche today might be replaced by new ones tomorrow. But Darly Solutions always keeps its finger on the pulse and offers you a quality combination of the latest technologies and reliable practices.
Conclusion
Medical Billing Software is not an option but a real need for medical institutions that wish to provide modern services and have automated tools for billing. Yes, the development and implementation of such systems can be costly, but in the end, clinics gain long-term benefits.
For the development and implementation of Medical Billing Software, you need a clear understanding of your institution’s needs and a reliable provider. By choosing Darly Solutions, you get a comprehensive service that covers all stages of deploying this type of platform.
Ready to start collaboration? Contact our team manager to launch the project!


COVID-19 marked a turning point for digital health. In fact, it made mobile medical apps mainstream in healthcare. According to Statista, as of 2025, the Google Play Store had over 36K healthcare apps, and the Apple App Store had over 35K. These apps cover telemedicine, fitness, wellness, mental health, nutrition, and pharmacy delivery, competing for users' attention and digitalizing the traditional healthcare industry.
Since development isn't just about coding, it requires complex regulatory navigation, technological and market demands, and strategic investment.
The cost of developing a health app will vary depending on what kind of app you want to launch. In fact, all types of eHealth apps, from telemedicine, fitness and wellness, mental health, and nutrition planning to pharmacy delivery apps — are getting great traction in the market today.
In this article, you will learn what affects the cost of developing a healthcare mobile app.
Healthcare Apps Market Overview
The mHealth app sector demonstrates skyrocketing growth driven by evolving healthcare delivery models. According to Grand View Research, the global healthcare app market will grow at a 14.9% CAGR through 2030. This growth is due to increased smartphone use for health tracking, the rise of AI assistants, and a demand for remote, patient-centered care.
Advantages of Developing a Healthcare App
Digitalization and automatization run the world, and healthcare thrives here the most. Since patients can now reach doctors with a few clicks, digital monitoring and telemedicine cut care costs by 25%.
About 63.4% of U.S. adults use mobile health apps, with many relying on them daily for fitness and wellness tracking. Additionally, a survey showed that 59% of participants have 1-3 health-related apps, which highlights even more significance of healthcare apps.
And the benefits don't end here. Dive with us into some of the other top benefits of healthcare apps:

Improved Patient Engagement
mHealth apps lead to better patient outcomes. With remote monitoring and reminders, they provide direct communication with providers and offer personalized health management tools.
Patient Customization and Tailored Treatments
Custom mobile apps streamline access to patient records. They help doctors create personalized treatment plans, improving outcomes and patient-provider relationships.
Medication Adherence Support
Medication reminders and tracking tools within these apps promote adherence, empower patients, enable timely provider intervention, and improve the management of chronic conditions.
Health and Fitness Tracking
Real-time data fosters proactive wellness and motivates users to achieve their health goals. Sharing this data with healthcare providers facilitates personalized care and timely interventions.
Analysis of Patient Behavior
These apps track patient behavior, including mood, medication use, and lifestyle choices. Real-time feedback lets doctors adjust their plans. Improved communication boosts patient engagement and outcomes.
Real-Time Global Collaboration
These apps break down geographical barriers and enable global healthcare teams to collaborate on personalized treatments. Continuous patient monitoring enables prompt intervention, fosters proactive healthcare, and raises global care standards.
Emergency Services Integration:
Healthcare apps with emergency services let users quickly contact help, share their location, and get help in emergencies. This approach improves response times and can save lives.
Reduced Diagnostic Errors
mHealth apps enhance diagnostic accuracy and patient safety. Intelligent tools support better decision-making, while predictive features help identify potential drug interactions and other adverse events.
Secure and Convenient Payment Options
Integrated payment gateways enable seamless transactions via credit/debit cards or PayPal. Automated notifications and easy access to payment history streamline billing and enhance patient satisfaction.
Efficient Data Management
Using AI and blockchain in mobile health apps improves data management, streamlines processes, and enhances doctor-patient communication. This approach leads to more personalized treatment and better health outcomes.
Types of Healthcare Apps and Their Development Cost
In this section, we'll look at the average cost to build a healthcare app across various categories.

Telemedicine App
Telemedicine is a synonym for modern healthcare. Now, healthcare professionals are at the fingertips and available from the comfort of home. From virtual consultations to video calls, the possibilities are vast.
Check for key components, cost, and timeline of the app deployment below:

Health and Wellness Tracking App
Given the vast and growing market, launching a wellness app is a promising venture. Look at the success of Headspace and Calm. They help many users find a sense of calm every day. Wellness apps typically include features like meditation, mindfulness practices, and productivity tools. With AI-powered nudges, you can help users stay mindful and re-energized.
Inspect the key aspects, budget requirements, and timeline for deploying the app below:

Medical Networking App
These platforms harness the power of the Internet to foster connections and collaboration. Healthcare providers can use these apps to expand their knowledge and share important information with respected colleagues.
Below, we've listed the app's features, financial estimates, and launch timeline:

E-prescription Apps
E-prescription apps are reshaping the prescription process, blending security with efficiency. They allow healthcare professionals to prescribe precise dosages, which pharmacies receive in real-time. This seamless flow ensures that medications are delivered right to patients' homes, making healthcare as easy as a tap on the screen.
Here's a detailed look at the app's features, cost projections, and expected timeline.

Hospital & Clinics Management Apps
Hospital and clinic management apps simplify administrative tasks, improve resource allocation, and boost overall efficiency in healthcare settings.
Below, we've detailed the app's features, pricing estimates, and launch schedule.

Chronic Disease Management Apps
Chronic disease management apps help users track symptoms, manage medications, and communicate with healthcare providers.
Take a closer look at the app's features, estimated costs, and projected timeline.

Appointment Scheduling Apps
Healthcare appointment scheduling apps make booking and modifying appointments easier, which improves patient satisfaction.
The app's primary functions, projected costs, and deployment timeline are listed below.

EHR/EMR Systems
Modern healthcare demands secure digital record systems. Blockchain EHR platforms protect sensitive patient data while facilitating doctor-patient communication. Smart contract automation streamlines medical workflows.
Check the app's core functionalities, expected expenses, and rollout schedule below.

Remote Monitoring Apps
Remote monitoring apps provide real-time insights into patients' health metrics, empowering healthcare professionals to act swiftly. This seamless connection ensures timely interventions, making healthcare more responsive and effective.
See the app's features, financial estimates, and launch timeline below.

Medical billing and coding
Medical Billing means submitting and following up on claims with health insurers to get paid for services by healthcare providers. It also includes verifying patient insurance, processing payments, and managing accounts receivable.
Medical Coding turns healthcare diagnoses, procedures, and services into universal alphanumeric codes. Accurate coding is crucial; it directly impacts billing accuracy and claim approvals.
If speaking to the real-world case, the hospital tracked underpayments and payer performance by implementing the billing system, boosting patient collections from 5% to 22-26%.
Key Features of Medical Billing Software
- Patient Record Management.
Efficient management of patient records eliminates manual filing and ensures quick access to necessary information.
- Medical Coding Automation.
The software supports standardized coding systems like ICD-10 and CPT to automate the coding process and reduce claim denials due to errors.
- Payment Processing Integration.
Integrated payment processing capabilities allow secure online payments via various methods, enhancing patient convenience.
- Financial Performance Analytics.
Tools for generating reports on collections, rejections, and overall financial performance help healthcare providers analyze their revenue cycle.
- Electronic Health Record Synchronization.
Seamless integration with Electronic Health Records (EHR) systems consolidates data accurately, improving workflow efficiency and reducing billing errors.
Steps in Developing Medical Billing Software
Developing medical billing software requires a strategic approach. It must balance technical complexity, compliance with regulations, and a user-centric design. This process involves planning, skilled development, and rigorous testing to meet healthcare standards.
Define Requirements.
Clearly outline the functionalities needed based on user feedback and technical specifications.
Software Development.
Engage a team of developers to create the software, focusing on design specifications, security considerations, and compliance with regulations like HIPAA.
Testing.
Conduct thorough testing to ensure functionality meets compliance standards and is free from technical issues before deployment.
Formula to Calculate Medical App Development Cost
The final estimate of your healthcare mobile app development cost relies on the duration of your project. However, you can calculate the approximate cost using the formula for the healthcare app development cost:
The hourly rate is the cost charged per hour of work, and development hours account for the total time used in the process.

Note!
The hourly rates depend on the skills and location of the app developers. If you have an offshore team, you might gain some cost advantages. Yet, skilled professionals might charge higher fixed prices. You must balance expertise and budget to get the best app development value.
Cost Per Feature in Healthcare App Development
The cost of healthcare app development is the cornerstone. Each added feature impacts the overall budget. For instance, user authentication can cost $2,000 to $5,000. Telemedicine features may cost $10,000 to $15,000. User-centric options, like appointment scheduling, cost $1,000 to $3,000 each. Strategic planning is essential to manage costs effectively.
Let's take a closer look at the price of each feature:

Cost Per Hour for App Development By Region
The hourly rate for healthcare app development isn't set in stone; it varies widely based on several key factors. They involve the app's complexity, the developers' expertise, their location, and the project's scope.
Here's a quick guide to typical hourly rates across different regions:
North America (USA, Canada): $100 – $250
The rates in North America are among the highest globally due to the high demand for skilled developers and the cost of living in major tech hubs like Silicon Valley. Senior full-stack developers can charge between $150 and $200 per hour.
Western Europe (UK, Germany, France): $80 – $200
This region has high rates due to a strong demand for skilled developers and a robust business environment. Countries like Germany and the UK typically charge between $22 and $90 per hour for developers, depending on their experience level. The average salary for software engineers in Western Europe ranges from $60,000 to $95,000 annually.
Eastern Europe (Poland, Ukraine, Romania): $40 – $100
Eastern Europe offers a competitive balance of cost and quality. The average hourly rate is lower than in Western Europe, with many skilled developers available between $24 and $46 per hour. With strong technical education and a growing IT workforce, Poland and Ukraine offer readily available development talent.
Asia (India, China, Philippines): $20 – $80
Asia generally offers the lowest rates for software development. However, quality can vary widely among developers. Rates typically range from $10 to $80 per hour. It is crucial to thoroughly vet developers in this region to ensure quality and reliability.
Australia and New Zealand: $80 – $150
Developers in Australia and New Zealand command higher salaries due to the high cost of living and demand for skilled labor. Average hourly rates range from approximately $50 to $150, depending on experience and specialization.
South America (Brazil, Argentina): $30 – $100
South America presents competitive rates with a growing pool of talented developers. Hourly rates typically range from $20 to $100, making it an attractive option for companies seeking cost-effective development solutions while maintaining quality.
Hidden Expenses in App Development
When planning a budget for mhealth app development, don't forget to account for these additional costs:
- Project Management: Usually adds 10-20% to the overall medical app development cost.
- Design: UI/UX design rates typically range from $50 to $150 per hour.
- Testing and QA: Costs generally fall between $30 and $100 per hour.
- Maintenance and Support: Ongoing expenses after launch are often billed at the same hourly rate as development.
Note!
These approximate figures may fluctuate based on your project's specifics and development team.
Legal and regulatory costs
Legal and regulatory healthcare app development costs can range from $5,000 to $15,000 annually. This covers compliance with key regulations like HIPAA in the U.S. and GDPR in Europe. These costs include fees for obtaining certifications, conducting privacy audits, and ensuring compliance with evolving legal standards. Developers must also consider the costs of data protection. They may need to consult lawyers to navigate complex regulations.
What Affects the Healthcare App Development Costs?
Healthcare software solutions come with different price tags. For example, an EHR system may cost $10K to $250K, while telemedicine platforms can range from $40K to $400K. What factors contribute to these costs? We're here to explain.
Scope and complexity
Healthcare app development costs hinge on project complexity. Advanced features like AI-powered decision support, analytics, and device integration drive up expenses and development timelines. Precise project scoping is critical: it minimizes unexpected costs and ensures optimal resource allocation.
Regulatory compliance
Protecting patient data via HIPAA compliance is non-negotiable, as it entails trust in healthcare services overall. However, it often comes at a cost: increased development complexity, higher expenses, and the added overhead of certifications impact both — budget and time to market.
Integration requirements
System compatibility drives up healthcare software development expenses. For compatibility and seamless data transfer, developers must invest substantial effort in connecting new software with legacy Electronic Health Record (EHR) and Electronic Medical Record (EMR) systems. The integration process becomes more complex when incorporating third-party services like payment platforms, telehealth tools, and laboratory information systems, dramatically increasing both development and testing costs.
Technology stack
Cross-platform software development multiplies costs. Creating separate codebases for web, iOS, and Android platforms can exponentially increase development expenses. Moreover, integrating cutting-edge technologies like AI and blockchain requires rare expertise, significantly inflating development costs.
Development team composition
Healthcare app development costs depend on the team structure. An in-house team may provide more control, while outsourcing to a third-party vendor can be more cost-efficient with proper management. Remember that specialized skills, such as cybersecurity experts and data scientists, are usually more expensive.
Design and user experience
Design determines healthcare software success. While a high-quality, user-friendly design may increase initial healthcare app development costs upfront, it drives better adoption and satisfaction in the long run. Features for disabled users will have higher design and development costs. Major expenses come from thorough research, testing, and iterative development.
Testing and quality assurance
The smooth operation of healthcare software depends on regular testing. In-depth testing for functionality, security, compliance, and performance raises healthcare app development costs due to the lengthy cycles involved. Feedback from real users during testing further raises the overall project expenses.
Maintenance and support
Healthcare software expenses don't end at development. Maintenance and post-launch support (e.g., bug fixes, updates, regulatory compliance changes) demand ongoing investment. Additionally, providing user support services adds to overall operational expenses.

These factors guide informed decisions on scope, technology, and resources for healthcare software development. Plus, they empower effective budgeting and cost management, often resulting in successful healthcare software development initiatives.
Best Practices for Cost-Efficient Healthcare App Development
Deployment of healthcare apps is an expensive process. Sometimes, it squishes the expenditures; software integration expenses range from $20,000 to $100,000, while regulatory compliance adds $20,000 to $80,000 to development budgets. These substantial costs necessitate strategic financial management.
Smart business owners seek smart moves to keep healthcare app development costs under control. Here are some options available in detail:
Opt For Cross-Platform Development Tools.
React Native and Flutter can cut your budget by up to 1.5 times through a shared iOS and Android codebase. In addition, source code from a cross-platform mobile app can be repurposed to create a web application.
Leverage Off-the-Shelf SDKs and Code Libraries.
Businesses can use existing solutions and customize them to fit their needs instead of building common features from scratch. Pick a ready-made option and modify it to fit your specific needs.
Consider White-Label and No-Code Solutions.
Branded and system-integrable off-the-shelf products provide a cost-effective way to roll out services like telehealth. This white-label product integrates with your digital systems, like practice management platforms. It lets clinics cost-effectively start telehealth services using no-code solutions.
Conduct Rapid Prototyping.
Before diving into full development, opt for prototyping. This stage can help validate your ideas and test the UI/UX while cutting unnecessary costs.
Employ a Multidisciplinary Team.
Hire a full-stack team that includes in-house talent in design, development, QA, etc. Clearer, more concise communication keeps mHealth app development costs under control.
Outsource Smart.
Outsourcing holds potential as a strategic solution yet demands careful evaluation before proceeding. Combining medical app development intricacies with cultural misunderstandings can produce a product that fails to fulfill expectations. The cost of healthcare app development in the USA mirrors its distinct challenges and established standards.
Involve in the Development Process From the Start.
One of the greatest mistakes is to hire an experienced team and then leave to manage themselves. Make the feedback a routine, and maintain communication with the development team throughout the process. If you lack time and material — hire a dedicated project manager. Make sure your reliable partner maintains regular updates with you.
Conduct Thorough Testing.
QA is on your development partner. Nevertheless, you can also verify stuff on your end. Early detection of bugs simplifies their resolution while keeping costs low. To prevent old errors from recurring, developers should conduct retrospective tests.
Implement DevOps Best Practices.
Without appropriate DevOps practices, developers lose valuable time. Automated DevOps systems allow developers to focus on writing code features rather than spending time on manual quality assurance and releases.
Optimize Maintenance Costs.
Long-term maintenance costs decrease when automated platforms track issues and collect user feedback.
Prioritize Features Wisely.
Start with core features before building a Minimum Viable Product (MVP), enabling market testing before further development.
Regulatory Compliance For Health Apps
Developing medical applications requires strict adherence to international data protection standards. These regulations safeguard patient information and ensure legal compliance across global markets. Here's a comprehensive breakdown of key regulatory frameworks:
1. European Union: GDPR (General Data Protection Regulation)
Coverage: Patient health records and personal data
Key Features:
- Mandatory data breach reporting within 72 hours
- Patient right to data access and deletion
- Requires explicit consent for data collection
Fines: Up to €20M or 4% of global revenue
2. United States: HIPAA (Health Insurance Portability and Accountability Act)
Coverage: Protected health information (PHI)
Requirements:
- End-to-end data encryption
- Access control mechanisms
- Audit trails for all data access
- Regular security assessments
Penalties: Up to $1.5M per violation annually
3. Canada: PIPEDA (Personal Information Protection and Electronic Documents Act)
Coverage: Private sector data handling
Key Requirements:
- Explicit consent for data collection
- Purpose limitation
- Data accuracy maintenance
- Security safeguards
Penalties: CAD 100K per violation.
Tech Stack For Healthcare App Development
Discussing the tech stack goes first, right before answering the ultimate question of how to develop a health app. Also, will the dev work blow the budget?
Since the health app's tech affects its performance, convenience, and company expenditures. Here are some common tech stacks for mhealth app development used by the Darly Studion team:
Programming Languages:
Java, Python, C#, C++, JavaScript, PHP, and HTML5.
The choice of specific language depends on the functionality you need. If the app stores and analyzes large data or uses AI, choose Python and Java for the backend and JavaScript for the front end.
Operating Systems:
Windows, macOS, Linux, and mobile Apple iOS or Google Android.
Here, we just need to choose a trustworthy provider with great support. We choose an OS with strong security and top performance.
Databases:
MySQL, Oracle, PostgreSQL, Memcached, and MongoDB.
To select the best database or a mix, contact a development team. They will evaluate your data type, volume, and request frequency to guide you in choosing the right database size and provider.
Servers:
Apache server and NGINX.
These two options lead the market, but their HIPAA compliance is most important to us.
Other useful tools:
- DevOps tools: GitHub, Jenkins, Selenium, Rollbar, or Bitbucket.
- Business tools such as Slack and G Suite — for communication and management.
- Tools like Google Analytics for tracking, Stripe for payments, and Elasticsearch for search enhance functionality.
- Cloud storage and hosting providers such as Amazon S3, Amazon EC2, or DigitalOcean.
Now that we've covered the technology stack for healthcare apps let's break down the next practical steps.
Design for Healthcare App Development: Best Practices
Creating effective healthcare applications requires meticulous attention to design principles that balance clinical utility with user experience. Studies show that 93% of physicians believe mobile health apps can improve patient care, while 80% of users abandon healthcare apps within the first 2 weeks due to poor design.
User Interface Design
Medical professionals spend an average of 4.5 hours daily interacting with healthcare interfaces. Design must accommodate the 15-second average attention span during critical care scenarios, with interfaces allowing task completion within three clicks or less.
Visual Elements
- Color schemes with a minimum 4.5:1 contrast ratio (WCAG 2.1 standards)
- Typography: 16px minimum for body text, 24px for headers
- Maximum of 6-8 core icons per screen to prevent cognitive overload
- 95% of users expect consistent branding across all touchpoints
Functionality Considerations
- Critical features accessible within 0.8 seconds
- The data visualization comprehension rate should exceed 90%
- Forms designed to reduce error rates below 1%
- 99.9% uptime for offline critical functions
Security Measures
- 2-factor authentication reduces breaches by 99.9%
- 256-bit AES encryption ensures the security of data at rest and in transit
- HIPAA compliance requires 72-hour breach notification
- Monthly security audits covering 100% of the codebase
Accessibility Features
- Voice commands with a 95% accuracy rate
- Screen readers supporting 40+ languages
- Text scaling from 100% to 400%
- Regional support for 25+ major healthcare markets
Performance Optimization
- Page load times under 3 seconds (Google's benchmark)
- Data sync completion within 5 seconds
- Maximum 5% battery drain per hour of active use
- 99% crash-free sessions rate
Testing Requirements
- Minimum 500 hours of user testing with healthcare professionals
- 100% compliance with ISO 13485 medical device standards
- Testing across 15+ device types and 5+ operating systems
- Weekly security scans covering 50+ vulnerability types
Key Metrics for Success:
- User Retention: Target 70% after 30 days
- Task Success Rate: Minimum 95%
- Error Recovery: Under 5 seconds
- System Response Time: Under 0.1 seconds
- User Satisfaction Score: Above 85%
Healthcare Application Development Steps
Crafting a custom medical software development service demands mastering five non-negotiable development stages:

Step 1. Shape the concept for your app
Before writing a single line of code, decode the fundamental value proposition, transforming your app from a mere download to a user's daily digital health companion.
Decode your audience's DNA.
Segment users by age, location, and average income. Analyze their needs to create a value proposition that challenges industry standards.
Conduct market research.
Identify the strengths and weaknesses of your target market. Benchmark against competitors and develop a unique value framework.
List selling points.
Create a comprehensive list of features and additional services that will appeal to your target audience and encourage them to choose your mhealth app.
Define your goals.
Clearly outline the objectives you want the app to achieve and align them with your budget for effective planning.
Step 2. Choose the monetization model
Basically, there are six monetization business models for healthcare apps, from freemium to paid-in-app. This aspect is pretty simple for healthcare providers who decided to build a healthcare app as another platform to sell their services.
Healthcare providers who use healthcare apps to sell their services will find this aspect straightforward because they don't need to generate revenue from the app, which functions as an additional tool. However, the question is a bit more complicated for owners of apps such as meditation or healthy lifestyle platforms.
Step 3. Create UI/UX design
In this development phase, UI/UX designers establish the app's functionality and visual design while managing platform branding when necessary. The most time-consuming task during this stage remains developing prototypes that include visual mockups for each app screen and user interaction.
Another crucial part of the design process is selecting fonts, color schemes, and button placement. mHealth platforms must prioritize responsive design across all devices while ensuring users can reach their goals efficiently.
Step 4. Build an MVP
Even if you lack the necessary funding to implement your ideas today, that doesn't mean you cannot begin developing your project. That's what an MVP is for.
MVP creation enables faster launch and collection of initial user feedback. As your app develops, you can raise more funding. This will help expand its capabilities. An MVP approach cuts financial risk since it requires less investment to test a product's viability before committing further.
Step 5. Collect feedback and update
Typically, at this stage, QA engineers perform another round of testing after developers deploy updates to ensure that there are no bugs and that project requirements match the results.
Timeline of Custom Healthcare Software Development Services
The timeline for custom healthcare software development varies according to the complexity, scope, and specific requirements. Let's explore the general phases involved.
Initial consultation and planning.
This phase starts by engaging stakeholders to clarify their needs and objectives. It then lays down the scope, key features, and deliverables, resulting in a high-level timeline and budget. The project team then defines roles and responsibilities. This process typically takes two to four weeks.
Research and analysis.
The research and analysis phase starts by analyzing market trends and examining competitors' healthcare software solutions. The next step is gathering insights through surveys and interviews with potential users. The technology stack, third-party integrations, and compliance requirements are evaluated at this stage to ensure thoroughness. This vital phase will take three to five weeks and lay a solid foundation for your project.
Designing phase.
The design phase usually spans four to eight weeks. At this phase, create wireframes and prototypes for key screens and user journeys to develop a user-friendly interface. Additionally, conduct a usability test. Every detail must shine.
Development phase.
This phase lasts 12 to 24 weeks. It focuses on building the software's core: the backend, the front end, and key features like patient records, scheduling, and billing. The backend includes the databases and APIs. The front end must be user-friendly. Plus, robust security measures are integrated, including HIPAA and GDPR compliance.
Testing.
Before release, the software undergoes a 6 – to 10-week testing cycle. This includes unit tests, integration tests, performance tests, security tests, and user acceptance tests, which help ensure the software performs well and is secure.
Deployment and training.
The deployment and training of your healthcare software will take three to six weeks. At this phase, developers ensure the software works well, that any early issues are fixed quickly, and that the app is user-friendly.
Must-Have Features of Healthcare Apps
The type and main function of a healthcare app dictate its features. Yet, there are the most common that mHealth apps share, whether for telemedicine, hospitals, or urgent care. Here are the essentials:
- Sign-up / Sign-in. While in-app registration might require hefty user details and time to figure everything out, the sign-in process should be swift and easy. For a smooth experience, allow users to sign in with their email.
- Doctors' and patients' profiles. Doctors' profiles should display their specialization, education, current workplace, and availability. Patients' profiles must include their medical history, prescribed medications, and other key health details to ensure a seamless interaction.
- Appointment management. The calendar feature helps doctors track appointments and allows patients to browse available slots to book visits. A seamless experience for everyone involved!
- Push notifications. Designed for both healthcare workers and patients, these features act as reminders for upcoming appointments and medication alerts.
- In-app chat. With in-app chat, users can easily connect with healthcare managers or doctors. It enables faster communication, making healthcare more accessible and efficient.
- Video consultations. The shift to video call appointments came as a safer alternative during the pandemic when in-person consultations posed higher risks. Now, this option saves time for doctors and patients and lowers the chance of spreading illnesses.
- EHR integration. Each medical visit or procedure adds to a patient's treatment history, stored in an EHR (electronic health record) system. Including an EHR system in your app is vital for delivering the best care and streamlining the process for future healthcare providers treating the patient.
- E-prescriptions. As consultations move online, doctors should also be able to prescribe medications digitally, which cuts time waiting in key and frees up doctors' time. Another benefit is that e-prescriptions are more secure and difficult to forge.
- Payment gateway. Paid medical services go hand in hand with in-app payments. Thus, opt for payment gateways that accept credit and debit cards, digital wallets, crypto payments, and other alternative methods.
- Ratings and reviews. Designed for patients, this feature simplifies selecting a trusted professional who fits their specific requirements.
Challenges in Healthcare App Development
Healthcare app development faces several challenges that can hinder progress.
Non-Compliance with the Law.
HIPAA and FDA regulations safeguard personal data and guarantee the safety of products. Failure to follow these rules leads to financial penalties and the erosion of trust. To ensure compliance and avoid penalties, businesses must consult legal experts.
Lack of Security.
Hackers can quickly access sensitive data, such as customer information or financial records, when business security systems fail. Businesses can suffer reputational damage and financial losses due to this. To prevent this, businesses must improve their security and work with tech experts.
Presence of Multiple Channels and Devices.
Multiple channels and devices present integration challenges since they operate on unique systems and protocols while meeting different requirements. Differences between technology standards and data formats trigger compatibility problems that need additional effort to fix.
Marketing and Launch Cost of Healthcare Application
Depending on scale and strategy, a healthcare app's marketing and launch costs can range from $5,000 to over $100,000. Key cost components include:
- Market Research: $5,000 to $15,000 for analyzing market needs and competition.
- Launch Campaigns: $5,000 to $100,000 based on scope and platforms.
- User Acquisition Costs: Cost per install (CPI) ranges from $1.42 to $3.75, varying by advertising platform (e.g., Google Ads, Facebook Ads).
Effective budgeting is essential for a successful launch and user engagement.
Business and Monetization Models of Healthcare Apps
Since healthcare thrives on digitalization, many people have at least one app on their devices. However, the competition for user attention takes high stakes. The question arises: How can we promote and monetize mhealth apps?
Below, we have listed some of the most common business and monetization models:
Freemium Model
The freemium healthcare app offers a basic version and charges for premium features like advanced health evaluations. This model promotes rapid market penetration and attracts a large user base. In the long run, it drives sustainable revenue by converting a percentage of free users to paid tiers.
Subscription Plans
Subscription models work best for healthcare apps offering ongoing value. Tiered pricing can include basic tracking features, fitness coaching or telehealth services, access to a library of health articles, and premium telemedicine services with personalized health plans. Before enroll this model, ensure its pricing reflects the app's unique value proposition.
In-App Purchases
Even though it has a complicated deployment architecture, it is an incredibly lucrative way to monetize the app. In short, this model helps to upsell extra features or content within the app. Thus, users can purchase in-app items such as extra lives in games, extra workouts in fitness apps, or pre-paid visits and prescriptions in mhealth apps.
Also, businesses often sell branded merchandise or partner with other brands via in-app purchases to promote themselves more.
Telemedicine Consultations
The pandemic marked the popular era of telemedicine. Now, many apps offer video consultations with subscription plans or pay-per-consultation fees. However, the healthcare specialists' credentials and licenses are the most important. They are the foundation of brand trust and revenue.
Advertising and Sponsorships
Healthcare apps monetize through strategic sponsorships and expert content. Targeted advertising creates win-win partnerships. It lets companies reach specific audiences and generate app revenue.
Partner with medical experts to create credible content, like articles and videos. This strategy will boost the app's credibility, expand its reach, and diversify revenue.
Pay-per-usage Model
The pay-per-usage model, common in SaaS, is now being implemented in healthcare apps. This cost-effective approach allows users to access healthcare resources and pay only for their actual usage, avoiding the commitment of a subscription. Which often results in user trust and brand loyalty.
These models can be mixed and matched depending on the target audience and specific functionalities of the healthcare app. However, first things first, robust business and monetization require a consistent content publishing strategy and tools to publish high-quality medical content regularly.
Healthcare App Development in a Nutshell
Indeed, healthcare apps are transforming digital health with more accessible and intuitive tools. From telemedicine and health trackers, the healthcare app development cost varies by type, scope, team, and overall business aim.
But the truth is one. Building a successful mobile health app requires strategic planning, research, and expertise in medical software development combined with a significant investment. This is especially true since medical app development costs go beyond initial creation, including planning, regulatory compliance, and ongoing maintenance.
Effective apps demand resource management and collaboration with experienced teams. A smart approach can help businesses develop impactful solutions that benefit both patients and healthcare providers.
Partnering with Darly Solutions enables companies to create healthcare apps that meet technical standards while delivering real value in digital health.
Build Your Healthcare Application With Darly Solutions
From market analysis to launch, Darly Solutions uses a strategic 5-step process to build high-quality healthcare mobile apps tailored to your audience. Follow us:
- Market & User Analysis: We help you understand your target audience (patients, doctors, etc.) and analyze existing apps to identify opportunities.
- Planning & Business Analysis: We collaborate with you to define the app's concept, business goals, technology, and resources, ensuring alignment with your strategy.
- Design & Prototyping: We design user-friendly interfaces and develop prototypes to validate requirements and gather feedback.
- Development & Testing: Using Agile methodology, we build and rigorously test the app in iterative sprints.
- Release & Support: We handle app store publication system integration and provide ongoing maintenance and support.
For now, don't settle for less. Darly Solution is here to help! Reach out today to discuss your project in detail.


In the U.S. HealthTech industry, time to market, data security, and regulatory compliance are non-negotiable. But even well-funded teams with in-house developers often find themselves in a quandary: they are overwhelmed by competing priorities, lack industry expertise, or can't move fast enough to meet release deadlines.
This article discusses how outsourcing helped a U.S. healthcare company build a clinical data monitoring tool faster, safer, and with tighter controls than an in-house team could have done. It also explores why outsourcing is often the more strategic choice in 2025.
The Project Context
The client is a U.S. HealthTech company with an in-house backend system that is already up and running. They needed to build a clinical data monitoring interface that would:
- Integrate seamlessly with existing infrastructure.
- Handle sensitive patient data under HIPAA.
- Offer a user-friendly dashboard for trial administrators and clinicians.
- Be delivered quickly, without disrupting the internal roadmap.
Their internal team was focused on core backend infrastructure. While capable, they didn’t have the bandwidth or specific expertise in data visualization and regulated interface design. The client needed a fast, compliant, and scalable solution—without hiring full-time.
Key point: This wasn’t a team that “couldn’t do it.” It was a team that didn’t have the right bandwidth or specialized roles at the right time. The result? Risk of project delays and regulatory exposure.
What an In-House Team Would Require
To build and maintain this type of clinical data monitoring system internally, a company would need:
- 2+ front-end engineers experienced in PHI-safe architecture.
- 1 UX designer familiar with clinical interfaces and dashboards.
- 1 DevSecOps engineer to manage secure infrastructure.
- 1 project manager with experience in HIPAA/FDA-compliant software delivery.
- Time and budget to recruit, onboard, and retain this team.
That’s at least 4–5 full-time hires. In 2025, hiring a senior developer in the U.S. costs around $160K–$190K annually, including taxes and benefits. Add recruitment time (8–12 weeks), onboarding, and the risk of team gaps—timeline quickly stretches beyond the planned release. Multiply that by 5 roles—and factor in ramp-up time—and total project costs could easily surpass $400K over six months.
Why the Company Chose Outsourcing
Rather than overburden their internal roadmap or spend months assembling a team, the company partnered with Darly Solutions, which already works with U.S. healthcare clients. Within 5 business days, a remote team was onboarded, including:
- Frontend developers with clinical data experience.
- A UX designer with multiple HIPAA-regulated projects behind them.
- A project manager and tech lead who took full ownership of the delivery.
They worked within the client’s architecture, maintained full transparency, and delivered a production-ready solution ahead of schedule. The client retained control over infrastructure, access, and IP without being pulled away from their core priorities.
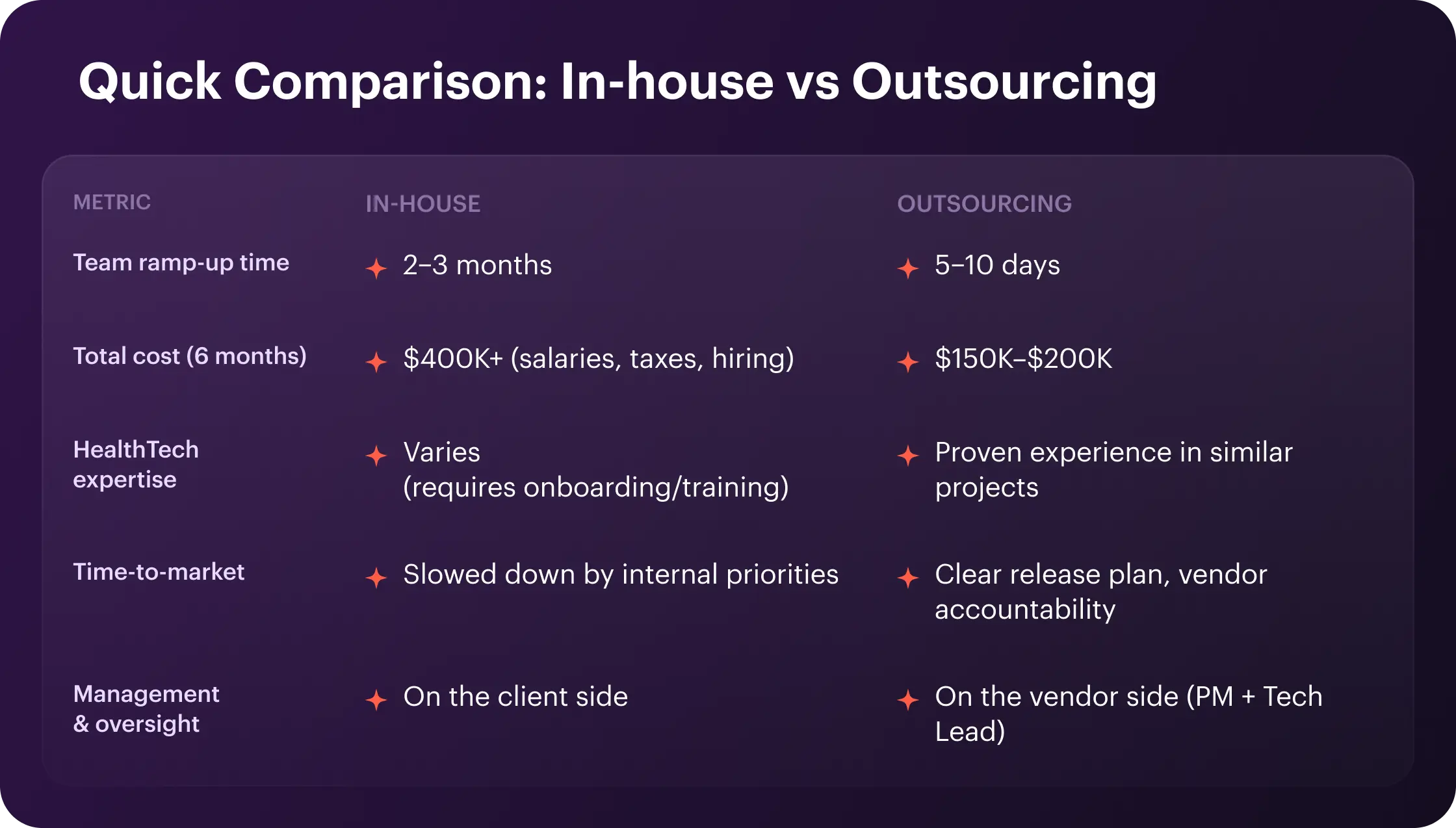
Security Concerns: The Most Common Objection
One of the most common objections we hear from HealthTech companies in the U.S. is:
“If development happens outside our walls, how can we be sure our data and infrastructure are truly protected?”
The concern is valid, especially when you’re dealing with highly sensitive health data, clinical trials, and strict U.S. regulations.
In a recent conversation with a HealthTech executive, we heard this exact fear. His company works with external teams and handles massive volumes of sensitive patient data. His worry wasn’t about code quality or delivery speed—it was about not having full visibility and control over the systems and people handling that data.
He shared:
“Our internal teams understand exactly how and where data moves. But, it's harder to feel in control when we involve external partners, even with NDAs and contracts. And if something goes wrong—who's ultimately responsible?”
But Here’s the Reality: Control Comes from Process, Not Geography
The key misunderstanding here is that in-house automatically equals “safe”, and outsourced means “risky.” That’s not true.
Security in HealthTech doesn’t depend on where the team sits. It depends on how access is managed, how infrastructure is configured, and how compliance is enforced.
When working with an experienced HealthTech outsourcing partner, companies can enforce:
- Role-based access controls (RBAC) with audit trails.
- Environment isolation: dev/staging/production strictly separated.
- On-premises or private cloud deployment, under your control.
- Regular compliance checks aligned with HIPAA.
- Source code ownership and internal code reviews.
- Strict NDAs, DPAs, and custom security policies in place.
In fact, a structured outsourcing setup often introduces more formal security governance than internal “trusted” processes that lack documentation or auditability.
The Results
With outsourcing, the client:
- Delivered a fully compliant monitoring interface integrated into their existing system.
- Avoided delays tied to internal hiring or overcommitment.
- Retained full IP and infrastructure control.
- Passed HIPAA audit without revisions.
- Saved $250K+ compared to in-house staffing.
- Released the product to production 3 months earlier than initially projected.
And they did all of it without overloading their internal team.
Final Thoughts: Outsourcing as a Strategic Enabler
Outsourcing isn’t a workaround—it’s a way to move faster without compromising quality or control. For HealthTech companies, it can be the difference between hitting a clinical release window and missing it by quarters.
It's not about replacing your internal team. It's about unlocking execution capacity when you need it most—supported by specialists who know your industry and your risks.
Outsourcing done right gives you:
- Faster time-to-market.
- Lower delivery costs.
- Full security and compliance.
- Experienced teams on demand.
- Predictable outcomes with shared accountability.
👉 Want the Technical Details?
Explore how we designed and delivered the monitoring solution in the full case study.


With the global aging population and the rise of chronic diseases, the remote patient monitoring market is booming as ever. From 2023 to 2024, it grew from $30.97B to $36.31B. And it won't stop here. Insider Intelligence predicts 70.6M US patients will use software for remote patient monitoring by 2025.
We can't overstate the importance of remote patient monitoring software. Such apps improve access to care, reduce hospital readmissions, and help save up to 60% on hospital visits, which results in higher-quality treatment in the comfort of patients' homes.
And benefits don't end up here. With ongoing digitalization via IoT and modernization of the healthcare system, don't wait for the best time for remote patient monitoring software development. The best time is now.
We've detailed remote patient monitoring apps below and covered their benefits, architecture, and top examples. You'll also see how Darly Solutions crafted an app for the health tech company. Read on, and stay tuned.
RPM monitoring software—is a digital tool for wearables, mobile apps, and medical devices that collects, analyzes, and shares patient data with medical personnel. Heart rate, blood sugar, and oxygen levels are among the most vital metrics. RPM software scores help catch health issues early, manage chronic conditions, and aid post-operative recovery.

How remote patient monitoring software works
From heart rate to blood glucose, each RPM system is designed to monitor a specific aspect of the body. However, elements included in any remote patient monitoring software development are typically the same. This is how the RPM system works:
- Collects and exchanges data.
Once calibrated, the devices send the data from the patient to the provider. The devices must have a Wi-Fi or LTE adapter for successful transfer. The data can also be sent via Bluetooth to IoT mobile apps via RPM devices. - Centralizes storage.
The provider securely stores the data collected from various sources, including patient devices, analytics systems, and e-medicine.
- Analyze.
The data is processed using advanced AI for management and analytics. Alerts are sent to caregivers, providers, and patients as needed, per their preferences. - Broadcasts.
Remote monitoring systems become telemedicine platforms when integrated with communication features like video conferencing, simplifying doctor-patient interaction.
- Sends emergency notifications.
When doctors identify health issues requiring daily monitoring, they oversee the data collected by the RPM system. Notably, it can notify emergency services if a patient needs urgent care. For non-urgent cases, patients can receive instructions for the next steps. However, HIPAA and similar regulations may restrict including sensitive patient information in certain notifications to protect privacy.
Why build remote patient monitoring software? Key advantages
Nevertheless, the RPM is part of the broader automation revolution; it has universal healthcare benefits overall. Let's examine the main of them:
Better access to health services
With remote patient monitoring software, medical services have no geographical boundaries. Patients can get timely medical attention at home and manage their health, fostering a greater sense of control under health conditions.
Improved patient outcomes
A study found that RPM cut hospital admissions for chronic care complications by 19% to 41%, which results in improved patient outcomes.
Cost-effective care with reduced readmissions
The average cost of hospital readmission is about $15,200, which makes the prevention of readmissions through remote patient monitoring software financially beneficial for both patients and providers. Even more, it is a well-established fact that early detection generally translates to lower healthcare costs.
Better client engagement and satisfaction
Over 94% of patients are satisfied with RPM's care. It sparks their curiosity about their health and boosts engagement. Such an increased sense of involvement often inspires commitment to treatment plans.
Early detection and timely intervention
The CDC reports that RPM can cut chronic disease complications by 40%. This highlights the need for swift intervention to reduce health risks.
Components of remote patient monitoring software
There is no one-fit RPM soft, as it differs in nature. However, each patient monitoring system generally has 3 to 5 basic components. Let’s delve into them:
Personal monitoring devices
From continuous glucose and heart rate monitors to blood pressure cuffs, digital scales, and peak flow meters.
Patient-side mobile applications
Prioritize user experience, making it easy for patients to access their health data. Additionally, they offer features like medication reminders and secure chats with healthcare providers.
Cloud database
Cloud repositories allow healthcare providers to store large patient data securely. They are scalable and accessible, adapting to growing datasets for long-term monitoring.
Hospital-side web app
These applications are part of hospital management software. They ensure compliance, enable integration, and support decision-making. Additionally, they offer reporting, notifications, and analytics to improve patient care.
Other modules
These comprise decision support systems, reporting tools, notification systems, and analytics platforms.
Essential features in remote patient monitoring solutions
Here are the essential features of a remote patient monitoring (RPM) solution:
Real-time tracking of patient vital signs
Wearable sensors, fitness trackers, blood pressure monitors, and glucose meters perfectly gather and handle real-time health metrics. Then, this data is sent to healthcare providers and added to Electronic Health Records (EHRs) for timely interventions and informed decisions preventing complications.
Intuitive interfaces and user-friendly features
Machines must be easy to set up, a breeze to wear, and simple to operate. Meanwhile, patients should access their data effortlessly through a smooth web or mobile app to track their progress. This connection allows seamless communication with healthcare providers, ensuring everyone's on the same page.
Accessibility features
Ultimately, create a system with all users in mind. Consider accessibility guidelines like WCAG and CVAA to pave the way for inclusive innovation. Encompass voice control for effortless data entry, navigation, and text-to-speech features to support people with dyslexia and other disabilities. Moreover, a patient-first design shines with screen reader compatibility, high-contrast modes, and a crystal-clear interface.
Personalized risk alerts and reminders
For swift and customizable alerts, the RPM system must adjust thresholds. For example, alerts can be sent when vital signs fall outside preset limits. This enables timely intervention to reduce the risk of adverse events.
Safe data transmission and storage
Patient data security is a top priority in remote patient monitoring software development. Thus, apps must comply with all regulations like HIPAA, as they protect the privacy and security of patient data and save from hefty fines.
Smooth EHR integration
EHR integration allows the automatic transfer of RPM data, giving healthcare providers access to complete patient histories for better decision-making and outcomes.
Reports and analysis of patient health data
Advanced analytics and reporting in remote patient monitoring software development provide valuable data insights for healthcare professionals (for data-driven decisions) and patients (to motivate healthier choices).
The architecture of a remote patient monitoring system
Remote health monitoring systems are designed with a multi-layered architecture. Basically, it has five core components that enable uninterrupted data flow within the system. Let’s break into the point of the whole structure:

Smart-connected sensors for health tracking
The sensor layer comprises remote monitoring devices such as EKGs, sleep trackers, smartwatches, and blood pressure monitors. Then, they transmit this data to the dedicated mobile app via Bluetooth or to the cloud via the Internet.
Patient interface
Patient-facing RPM apps collect real-time health data from connected medical devices, allowing manual entry of symptoms and medication intake. RPM apps often include data visualizations for tracking health trends and may have integrated telemedicine features, such as video conferencing for appointments, follow-ups, prescriptions, and virtual consultations.
Cloud RPM server
Cloud services form the core of RPM systems, providing secure storage, processing, and data analysis from devices and the RPM app. This engine also integrates with EHR systems to access patient health information (PHI) in FHIR format. It can identify trends, such as early signs of complications.
Medical staff dashboard
Patient data flows bidirectionally between the medical staff interface and the cloud RPM server, enabling effective management by care teams.
- Data visualization module.
Via charts and graphs that show trends in vital signs, medication adherence, and other data, the module gives providers a 360-degree view of the patient. - Alert management module.
The system promptly alerts clinicians to critical situations and device failures in real-time. - Reporting module.
The module generates custom reports on patient data, which hugely help track progress and gain insights over time. - Communication module.
This module has two-way messaging, video chat, and/or telephony integration and is made for secure, remote communication between clinicians and patients. - Appointment management module.
This module handles appointment scheduling and patient-provider communication, allowing both patients and providers to request appointments.
Depending on the organization's needs, a doctor-facing RPM interface can include other modules, such as patient management, care plans, and patient education.
Admin web panel
A key part of the RPM architecture is a control dashboard. It helps with admin tasks like configuring roles, managing patients, and setting alarms.
Remote patient monitoring software development: Key steps
Once you have a clear idea for your software product, find an experienced dev company to implement it. When contacting your tech partner, you don't need detailed software requirements. A high-level understanding of the functionalities is enough to get started for any custom healthcare software development services stages. Let’s break them down:

Step 1: Requirement collection and analysis
The process starts by refining your product vision. Then, define project goals based on the health conditions your RPM solution will address. Your team will then identify core functions, pick the best tech stack, and plan the app's architecture. If integration with systems like EHRs is required, your tech partner will ensure compatibility.
Step 2: Outlining security and compliance requirements
Remote patient monitoring software must follow HIPAA and FDA rules. The development team implements audit trails, encryption, secure cloud storage, and APIs for secure communication to ensure data security and privacy. They also define a testing strategy for the pre- and post-production phases.
Step 3: Prototyping and design
To create an intuitive, user-first staff interface, UX/UI teams conduct user research to define user personas and journeys. Based on this research, designers create a prototype reflecting both the initial vision and user needs, gathering feedback on the user experience. The team prioritizes a clean, engaging, and accessible design. Based on feedback, they will refine the prototype and send the final designs to the dev team.
Step 4: Development and integration
Tech experts will use best practices to develop your RPM system iteratively to meet regulatory compliance. This work may include front and backend components, patient and doctor apps, and integration of medical devices.
Step 5: Testing
When it comes to RPM development—thorough software testing is as important as the development itself. After testing, developers should prioritize IoMT device compatibility. They must also ensure smooth integration with the RPM system for the most stability.
Step 6: Ongoing improvements
After deployment, the dev team monitors and tunes the RPM system to meet business and tech needs. They provide training and support for patients and healthcare professionals.
Beyond monitoring and troubleshooting, your tech team will prepare a roadmap for software updates. This will enhance the system's features and security in the future.
RPM Software Deployment: Challenges and Practical Solutions
Let us explore the most notable challenges organizations encounter while deploying their RPM.
Regulatory compliance
RPM's compliance with HIPAA and GDPR relies on strong data security and privacy. It must meet standards like ISO 27001 and IEC 62304 for this.
What to do:
- Develop a comprehensive compliance framework according to all requirements like HIPAA, GDPR, FTC (Federal Trade Commission), FDA regulations, and more.
- Conduct regular audits and assessments outlining clear policies and protocols for staff.
- Provide ongoing staff training to ensure they are aware of their responsibilities.
Data security and privacy
Healthcare organizations handle sensitive patient data (vitals, medical history, personal details, reports, treatment plans). Unauthorized access poses the risk of data breaches and subsequent fines that could total millions of dollars.
What to do:
- Use encryption techniques of RPM-collected data, telehealth appointment recordings, and other sensitive patient health data.
- Implement strong authentication and role-based access.
- Regular audits and security assessments.
- Conduct employee and patient training.
- Adopt role-based access control (RBAC)
Technology integration and compatibility
Outdated systems may lack compatibility, hindering integration and impacting data accuracy and security. Integrating EHR and clinical systems can also be difficult, affecting data sharing and patient care. Ensuring interoperability for seamless data exchange adds another layer of complexity.
What to do:
- Assess current infrastructure compatibility.
- Follow interoperability standards and protocols.
- Adopt HL7 and FHIR standards.
Cost-benefit analysis
RPM implementation presents a cost-benefit challenge for healthcare organizations. While offering benefits like improved outcomes and enhanced care, the substantial upfront investment in hardware, software, infrastructure, licensing, staff training, regulatory compliance, and data security must be carefully weighed.
What to do:
- Conduct thorough cost assessments.
- Estimate ROI and potential cost savings.
- Strategically allocate resources.
Data precision and accuracy
Inaccurate data transmission from RPM devices (e.g., wearables) poses a significant challenge, potentially leading to misdiagnosis and compromised treatment. Several factors can affect data accuracy, including device calibration, signal interference, network issues, and device quality.
What to do:
- Choose quality sensors and wearables.
- Regularly calibrate devices.
- Implement quality assurance measures.
Lack of patient engagement
Some patients fear switching to modern healthcare and its tech just because they are used to in-person hospital visits. Thus, using the devices, checking vital signs, and messaging the doctor may be hard for the patients.
What to do:
- Prioritize a user-friendly interface.
- Craft tutorials for device usage and RPM data analytics interpretation.
- Incorporate gamification elements (e.g., badges, progress tracking) to incentivize engagement.
- Bridge language barriers for diverse patient populations by providing support in multiple languages.
RPM software development cost
The cost of developing Remote Patient Monitoring (RPM) software varies based on complexity, features, and the development team's location. Here’s a breakdown of the estimated costs associated with RPM software development:
- Basic RPM application ranges from $50K–$70K.
- Standard RPM software ranges from $100K–$400K or higher, depending on the specific requirements and features.
- Costs can be $500K or more for advanced solutions with complex systems and integrations.
Both building an in-house tech team and outsourcing software development come with significant costs: salaries/recruitment expenses versus hourly rates and vendor fees. Without proper research, you risk overpaying for a software solution—whether through in-house hiring costs or outsourcing fees—or settling for a product that doesn't meet your requirements.
To calculate the precise budget for your RPM software development idea—please fill out this form. We will contact you shortly.
Best RPM software
Here are some popular remote patient monitoring use cases that might inspire you for your own:
CoachCare
CoachCare was founded over a decade ago, now supports over 3,000 organizations, and serves over 150,000 patients. Boasting a remarkable RPM, it claims a success rate exceeding 95%. It advocates for RPM coverage and collaborates with groups like CMS and AMA. CoachCare's tech lets patients log vital health metrics via an app. Its simplicity boosts engagement. Experts recognize its support of the healthcare industry.

Healee
Healee is a health tech company founded in 2017, now handles over 700,000 visits per month, both onsite and virtual, and supports 5,000 physicians across 200 clinics. With EHR, e-prescription, and billing integrations, the Healee platform streamlines healthcare delivery in wellness, mental health, chronic care, and women's health.

Doctolib
Founded in Paris in 2013, Doctolib is a top healthcare booking platform. It serves over 400,000 providers and 50 million users. It handles 70 million monthly bookings in France, Germany, and Italy. It offers appointment scheduling, telemedicine, and patient messaging. These services reduce missed appointments by 60% and save doctors 1.5 hours per week on administrative tasks.

Senseonics
This company revolutionizes blood glucose monitoring. The system features a sleek, removable transmitter and a sensor expertly implanted under the skin by a healthcare pro. Connected to a mobile app, the sensor offers real-time insights, alerting patients through their smartphones or smartwatches when their glucose levels are too high. Sharing data with healthcare providers and family members becomes a breeze, ensuring optimal treatment strategies.
Currently, around 6,000 users benefit from the Eversense CGM system. By 2025, Senseonics aims to double that number.

Teladoc
Established in 2006, this Hoboken, New Jersey-based powerhouse is revolutionizing healthcare. With an extensive network of licensed professionals, HRS proudly claims the #1 spot in KLAS’ ‘Top Remote Patient Monitoring Companies’ from 2020 to 2023.
HRS offers its innovative PatientConnect platform, featuring over 90 tailored RPM plans for healthcare providers. Beyond monitoring, HRS embraces holistic care, providing behavioral health services like therapy and psychiatry, ensuring a comprehensive touch on every aspect of patient wellbeing.

Improving patient outcomes with RPM software: A case by Darly Solutions
In particular, the health tech company approached us about remote patient monitoring software development. They faced challenges with patient tech literacy, especially among the elderly. There was a risk of data overload for providers. Patient engagement was inconsistent. There was a need for system integration, like with EHRs. Plus, they had to ensure data privacy and security (HIPAA compliance).
Since the deadline was tight and there were a lot of high-precision requirements—we created a detailed plan for the project, assigned UX/UI design, web development, QA, and project management tasks, and pinpointed the tech stack.
Technology stack
We understood that choosing the right technology stack was crucial for success. After thorough consideration, we selected:
- Angular: For building dynamic web applications.
- HTML/CSS: For structuring and formatting the user’s interface.
- Docker: To streamline deployment through containerization.
- ngRx: For effective state management.
- TailwindCSS: To enable rapid UI development.
- NGX Pagination: For efficient handling of large datasets.
- JSON: For smooth and efficient data transfer between client and server.
Our efforts paid off. We launched the product on time, meeting all design, functionality, and quality standards. Our client now has a competitive product that is well-placed to thrive in the innovative telemedicine sector.

Read the details of the case here.
Wrapping up
Rising public interest, health concerns, and tech advances drive the RPM market to new heights in solutions and revenue. As we noted earlier, these technologies enable 24/7 health monitoring. They also provide remote populations with access to quality treatments.
Doctors, nurses, and other healthcare staff should focus less on routine, manual tasks in the next few years. They should focus on saving lives and providing treatment, which RPM can support perfectly. It can greatly reduce burnout and ease stress on global healthcare systems while driving market share to higher results and stakeholder benefits.
This is a great time if you're considering developing your RPM solution.


In recent years, mental health has taken center stage globally. Currently, approximately 792M people globally have mental issues and lack access to traditional therapy due to financial constraints or societal stigma. The best way to solve the issue — is to go digital. That is where mental health app development comes into play. It cuts costs and makes mental health available to everybody around the globe.
As to the market, in 2024 alone, the app market saw expansion to approximately $7.38B. In a decade, forecasts promise growth up to nearly 10% annually, scorching $17.52B.
If you are ready to build a new solution — now is the perfect time to start. Below, we will explain how to develop a mental health app, share standout mental health app ideas, and highlight key factors to keep in mind.
Why mental health apps are in demand
Even though people have faced mental disorders throughout the entire history, only in recent years solving these problems become normal and generally accepted. And it won’t stop. Let’s numbers speak louder — according to 2019 alone, the global capitalization for the global antidepressant market was estimated at $11.67B. By 2027, the market promises to grow to a record $18.29B.
Of course, depression is not the only issue. According to the World Health Organization (WHO), there is a growing tendency for PTSD, anxiety, and OCD (due to economic instability, military conflicts, pandemics, as well as personal problems).
Additionally, the fast-paced world daily brings panic attacks, triggers, and burnout (prevalent among doctors, teachers, and IT workers). Youngsters are prone to issues, too; among the most “popular” — are low self-esteem and social isolation.
Financial constraints and a lack of free time put hefty pressure on those who need a traditional approach to addressing mental problems. Then, an in-person visit to a psychologist or psychiatrist becomes a real luxury. But what if there is a more efficient, accessible alternative? That’s where developing your mental health app comes in.
Business and monetization models of mental health applications
For mental health app development, the following monetization models have proven to be the most profitable:
- Fee for the services of real psychologists.
According to this model, the application acts as a platform, connecting users with professional psychologists, coaches, or therapists (similar to a marketplace with reviews, ratings, cost of services, and other attributes). In this case, the application earns the commission from each transaction (usually 15-30%). - Subscription-based model.
This model has a fixed fee for regular access to content and/or services for a certain period (month, year, etc.). If your app has diverse content and functions, offer multiple pricing models. This lets users pick a plan that suits their needs best. - Freemium.
These models give free access to basic functionality, with particular features to be paid. Usually, there are personalized recommendations, access to exclusive courses, advanced progress analytics, etc. - One-time purchase.
This model involves a one-time purchase of the application, after which the user has access to all its functionality. - In-app purchases.
Here, the basic functionality is available for free, but additional materials or services are paid (personalized plans, unique selections of tracks for meditation, etc.). - Ad-supported model.
In this case, app is free but includes built-in advertising (banners, videos, native advertising, etc.). At the same time, to improve the user experience, you can offer an option to turn off ads for an extra fee. - B2B model.
This model translates into you selling licenses to companies with internal programs to support employee mental health. - Selling merch.
This model focused on branded wellness merchandise promotion via scented candles, self-improvement guides, and mindfulness notebooks.
Top mental health apps on the market
Now, let's explore the most popular mental health apps. Perhaps they'll give you extra inspiration for your mental health app development project.
Headspace
Endorsed by the editors of the New York Times and 2.8 million users globally, Headspace is a product of the mental health company of the same name. Its core functionality includes meditations dedicated to improving sleep quality, relaxation, and cultivating mindfulness. They also offer courses on meditation, managing borderline emotional states, and more. Moreover, the platform has scientifically proven results in stress reduction and a user-friendly interface.

Calm
The Calm app is loved for high-quality content and a simple and intuitive interface. by 4.5 million (2023). And it is rightfully so. This app spins everything, from meditation sessions and effective breathing exercises to audio programs that are good for falling asleep faster. As for monetization, there is a free version with limited access. Full access to functionals is only available with a paid subscription.

BetterHelp
BetterHelp has over 2 million users and connects with licensed therapists via text, phone, and video. Patients must pay a fee to continue their subscription and can also volunteer to donate to others. This app goes far beyond mood issues. It covers complex disorders and symptoms, such as clinical depression and PTSD.

Talkspace
Talkspace provides online therapy with licensed therapists through a tiered subscription model (with health insurance coverage). Moreover, this app is ideal for managing medication treatment and has many formats for direct communication with psychotherapists (including cases of emergencies).

Moodfit
Founded in 2018, Moodfit has become the top mood assistant for more than a million people worldwide. It has personalization options, customized mood data analysis through visualization tools, and mood-improving recommendations. In addition, the app has cognitive-behavioral therapy exercises as a handy and entertaining way to deal with mental issues.

Woebot
Woebot is a free AI-driven bot founded by Dr. Alison in 2017. It is based on text format and has cognitive behavioral therapy methods. Initially, this software was intended for youngsters in college and graduate school, but today, people of all ages use it.

Sanvello
Sanvello, created by Dale Beermann and Chris Goettel, provides evidence-based CBT techniques and tools to support mental well-being. Since 2015, the app has offered free features and premium content through subscription or insurance.

Key components of a mental health app
Let's determine what mental health app features should be included by default.
Registration/authentication/authorization system
The main functionality of this system includes two types of registration: full-fledged, with the user’s email, and fast, through social networks (this is implemented through the OAuth 2.0 protocol, which is suitable for integration with Google, Apple, and Facebook).
For better protection of user data, use two-factor authentication and store hashed passwords. This can be done, for example, using bcrypt. Additionally, allow password recovery via email or SMS and register log-in/logout events for a data security audit.
User profile
Include the functionality for adding, saving, and changing personal information (name, age, mental health goals), maintaining the user’s activity history (exercise completed, courses, sessions with psychologists, etc.), and privacy settings (public/anonymous profile). Typically, profile data is stored in a relational database (PostgreSQL/MySQL); it is also necessary to set a clear separation between public and private user data.
Home screen and navigation
The home screen should feature a clickable menu, allowing users to update content based on their settings. You can also add push notifications (for example, using Firebase Cloud Messaging). As for the menu, place meditations, psychological tests, stretching, and yoga exercises in text, video, and/or audio format. You can also include real-time communication with specialists via text, voice, and video chats.
Use cloud platforms such as AWS S3 to ensure scalable content storage. If your application is media-rich — add media streaming via HLS.
Finally, localize content for users from different regions if you plan to maximize your target audience.
In-app payment system
If you plan to monetize your app through subscription payments or in-app purchases, integrate App Store and Google Play to process payments via the In-App Purchase API. You can deploy the web version via Stripe. Once everything is ready, provide access control based on the paid features.
Analytics and recommendations
Place functionality for tracking user progress and boosting their motivation (e.g., mood changes) and recommendations based on analytics. The latter makes sense to implement using machine learning models (e.g., based on TensorFlow).
What to consider before creating a mental health app?
The basic functionality of a mental health app goes far beyond making it popular and profitable. Therefore, to maximize your chances of success, consider the following factors before creating a mental health app.
Competitive environment
Usually, it involves the user interface, content accessibility, and the quality of the exercises/recommendations. Notably, the Calm application (sleep stories) and BetterHelp (online chat with therapists) are prime examples of such.
Analysis of bad ratings — matters too. In particular, users usually complain about the high subscription costs, lack of personalization, navigation problems, and negative experiences with customer support service. You can use it to make a competitive feature.
Target audience
Your target audience — above all. This can be young people (18-35 years old) who need an effective solution for stress management and improving sleep quality. Or the elderly might be searching for a more convenient professional in-home/palliative care format. Finally, it could be corporate clients who want to implement programs for the mental support of their employees.
Ultimately, user needs may vary. Based on the insights, determine the preferred content format (e.g., meditation, CBT, DBT, video sessions) and presentation style.
Regulatory requirements and user data privacy
The most common and comprehensive regulations are GDPR and HIPAA regulations, which govern the processing of personal data and medical information. To comply with them under the mental health app development process, you must implement data encryption (via SSL/TLS) and ensure transparent privacy policies.
Marketing strategy
To attract a broad user base, create a unique selling proposition. This can be achieved through AI diagnostics, integration with wearable devices via IoT, or simply offering a lower price than competitors. Next, point out the comprehensive marketing strategy. Select the right promotion channels: social media, partnerships with therapists, or advertising through user reviews. is essential for developing a comprehensive marketing strategy. Additionally, to retain users — regularly update content.
Testing and feedback
It’s better to subject an app with a diverse target audience to beta testing. To do so, find the first users who could be your potential consumers, gather feedback, and optimize the app based on their input.
Financial costs and ROI
Finally, estimate the project budget. It should include development, marketing, updates, customer support, and infrastructure maintenance. Given the costs, you must also estimate how long it will take till your project is profitable. It might be useful for future investors.
What are the main phases of mental health app development?
Now that you have so many insights at hand, you can start the mental health app development process. Let's find out how this happens in practice.
Ideation
First, define the problem. It is the mental health issues that trouble your audience and their goals. Obviously, your app should cover it. The solution might vary. It could reduce stress, help with sleep, or heal depression. Moreover, in the very first stage — conduct a competitive analysis. This will help identify niche leaders, find the target audience, and formulate a USP.
Planning
At this stage of the mental health app development process, you will already have enough information to determine the main functionality of your teletherapy application. Select a technology stack (or at least decide whether it will be a native or cross-platform solution), and clarify the business model. Based on this, you can calculate an approximate project budget.
Design
From now on, your mental health app developers can start creating prototypes and gradually turn them into a full-fledged design. Note that to develop mental health apps, you must use WCAG 2.0 guidelines, which ensure all users can access the app's functionality. Once the mental health app design is complete, test usability with real users to refine the navigation.
Development
The mental health app development process is divided into frontend and backend. The first includes the implementation of the user part of the software, and the second – everything that happens on the server side. As individual modules are ready, your mental health app developers will need to perform unit and integration testing to prevent difficult-to-fix bugs in the future.
Testing
Once the entire codebase is ready, QA specialists and testers will create test cases to ensure each function works correctly and the app performs well under high user load. This testing also ensures that all user actions within the app are secure and protect their privacy.
Release
Now that testing is complete, and all detected bugs are fixed, you can publish the application in the App Store and/or Google Play (your development team will first need to check whether it meets all platform requirements). After publishing, you can launch an advertising campaign to attract the first users, as well as set up tracking tools like Google Analytics and Amplitude to analyze user behavior.
Post-release support
At this mental health app development stage, you must check your application's speed and stability regularly. You will also need to update/expand its functionality once in a while and optimize what already exists based on feedback from real users. An equally important point is ensuring compatibility with newer versions of iOS/Android.
Challenges in mental health app development
Various challenges can arise during the mental health app development process. Let’s analyze them:
- Compliance with regulations.
Mental health apps often handle and maintain personal information, including medical data, which imposes obligations on you as a developer to implement GDPR, CCPA, or HIPAA compliance. - Balance between personalization and privacy.
While personalization — is a key feature of these apps, it sometimes conflicts with privacy requirements. To address this, implement advanced mechanisms for anonymizing user data, which will reduce the need to send sensitive information to the server.
- Evidence base.
The content provided by your app must be scientifically sound and effective for users. To do this, you should either accompany all your treatment plans with individual recommendations from real therapists or initially use approaches with proven effectiveness. - User retention.
Many users abandon apps after a few days of use, so your app may need additional retention mechanics (such as gamification and adaptive push notifications) that won’t make users feel guilty or overwhelmed. - Monetization efficiency.
Most users search for free or cheap health-related apps. At this point, you need to figure out the balance between user accessibility and the financial sustainability of your software.
How much do developers charge to build a mental health application?
The budget for developing a mental health app development depends on its complexity. So, we can't give exact numbers without first discussing your idea with your development team. But the approximate price ranges from:
- $140K for a teletherapy app.
- $70K for a simple mood-tracking app with self-monitoring features.
Back-end features, like a database and admin panel, are often overlooked in cost estimates. Developers typically include these in the overall pricing for mental health applications.
If you want to get an estimate of your project, please contact us.
Mental health app design: Best practices
Now, let's analyze several mental health apps (some of which have already been presented to you above) whose design has pleasantly surprised us. Maybe they will help you think better through your mental health app development process.
Headspace
This app is praised for its simple and minimalistic interface, with bright illustrations and smooth animations that literally "nudge" users to meditate with its help. It is also adapted for beginners and is generally perceived as intuitive. This approach to design minimizes anxiety in users and motivates them to meditate regularly.
Calm
The aesthetics of the Calm app lie primarily in the author's images of nature, a soft color scheme, and smooth animations. Together, they create an atmosphere of relaxation - that’s what you need to reduce stress. The app also stands out from its competitors with its "sleep stories" that help people with high anxiety fall asleep faster.
Reflectly
Reflectly's unique design uses artificial intelligence to offer a personalized experience. A clear, user-friendly interface, dynamic prompts, and mood analytics complement this. Together, these features make the app an ideal choice for audiences of all ages.

Daylio
Daylio's intuitive interface is accompanied by simple icons for tracking the user’s mood and activity. Moreover, all these application elements are easy. Developers ensured that performing target actions doesn’t take too long. The application also has a built-in report generator with visualization elements so that users can monitor their progress.

Happify
The Happify app has a gamified interface. It simplifies and informalises the process of improving the psycho-emotional state. The gamification principles here are based on scientific methods to improve mood. So, it does not add to users' cognitive load.

Mental health app ideas to succeed in 2025
In this section, let’s look through the most viral mental health app development ideas so you can pinpoint your project to success:
- Integration of AI.
AI assistants can help analyze moods and behavior patterns, give personalized recommendations on how to improve well-being, and remind them of any regular upcoming activities, like a daily mood rate system. - Social interaction.
This can be implemented via in-app groups of users with similar mental problems where they could share their healing experiences and receive mutual support. - Integration with wearable devices.
Through the IoT, you can analyze heart rate, assess stress levels, determine sleep quality, and create a common mental health map. - AR and VR tools integration.
It might be useful for relaxation (to enhance the immersion effect). - "Instant help".
Through the screen for quick access to ready-made materials and an online chat with a psychotherapist. - Content specially adapted for children and adolescents.
For example, these could be games for managing emotions or recommendations for teenagers on dealing with anxiety and stress; - B2B solutions for companies.
in particular, these could be psychotherapeutic assistance to prevent burnout.
Highlights of our experience in delivering healthcare solutions
Finally, we'd like to share our experience developing a mental health app. A client approached us to expand their services to the web, specifically to support small businesses recovering from the recession caused by the coronavirus pandemic. The objective was to create a platform to attract a target audience seeking health-related products and services.
For this project, we assembled a team of ten specialists. We chose Ionic and Vue.js for the frontend tech stack, with Laravel for the backend. The result was an online platform featuring a simplified login process, the ability to schedule and reschedule meetings between clients and trainers, an intuitive search for events and classes, role-based access, and an integrated payment system for online payments (covering group and individual courses, as well as event participation). We also implemented live session connections via Google Meet and Zoom. The solution was complemented by a clean, minimalist design with a calming color scheme, ensuring a pleasant and user-friendly experience.
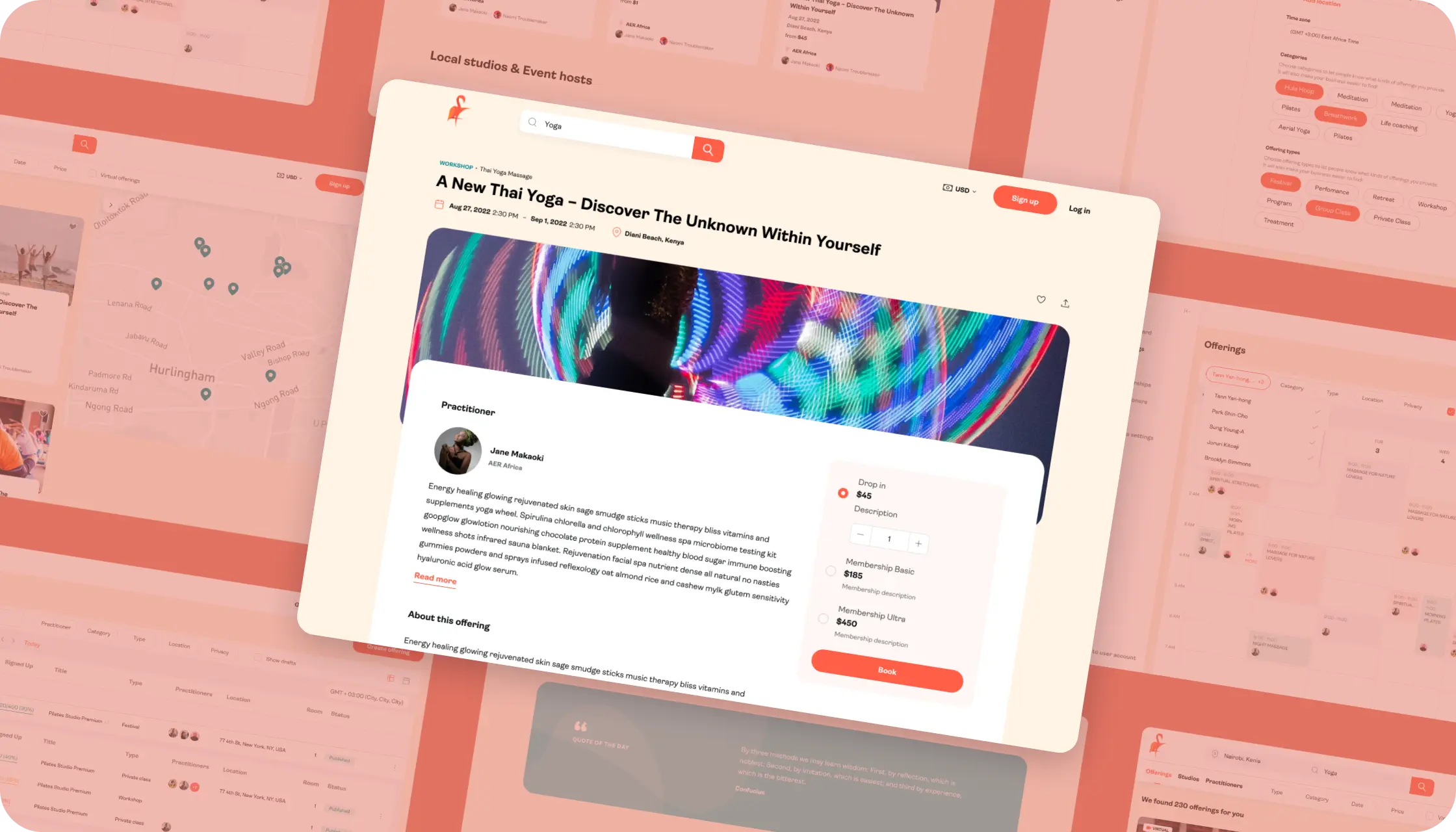
If you want to learn more about this project, please follow this link.
Final thoughts
With this comprehensive guide, you can confidently start looking for specialists who would bring your idea to life. Don’t go any further, as you are already in the right place! Just fill out this form, and our mental health app development team will contact you as soon as possible!


The future of healthcare is digital. In 2022 alone, the global patient portal market reached $2.9B, as the Grand View Research reports. By 2030, it’s projected to grow even higher—at a CAGR of 19.44%. This trend reflects how public and private healthcare organizations strive to digitize paper documentation and automate everyday business operations.
Indeed, the stakes in healthcare are high. Even minor errors can lead to incorrect diagnoses and worsen patients’ conditions. This is where patient portal software greatly minimizes errors, particularly those caused by human factors
Below, read on how to create a patient portal. We’ll analyze the target audience’s needs, dive into the most successful examples of its implementation, and examine the nature of the target audience's requirements.
What is a patient portal system?
An online patient portal is a web or mobile solution (usually for Android and iOS platforms) that gives patients access to medical records, helps schedule appointments in a few clicks, and easily communicate with healthcare providers at any time.
By automating the interaction between the parties via the patient portal, organizations can improve the quality of care while making their services more accessible and convenient for patients.
In particular, modern patient portal requirements are:
- Fast and secure access to their medical data and records with guaranteed privacy protection.
- High-quality medical services without the need to wait in long queues.
- A clear understanding of the treatment plan and progress.
Healthcare organizations instead aim to:
- Reduce their administrative costs – in particular, for maintaining paper documentation.
- Maximize personnel efficiency without the risk of burnout.
- Increase patient satisfaction through transparent interaction and remote patient monitoring.
- Comply with the healthcare regulations.
- Reach a new level of income by reducing expenses and attracting new patients.
That is why the patient portal system is the one-stop solution that, if implemented correctly, covers all the above-mentioned needs. This is typically achieved through the following features:
- Access to medical records (including medical history and test results).
- Appointment booking (with the option to select the date, time, and doctor).
- Online consultations (for example, via video calls and chats with doctors).
- Repeat prescription orders (automatic issuance of electronic prescriptions and reminders for refills).
- Online bill payment.
- Personal data management (including patient contact information).
- Push notifications (reminders for upcoming visits, tests, vaccinations, etc.).
- Educational materials.
- Feedback tools (surveys for patient satisfaction and forms for submitting complaints, etc.).
Types of patient portals: Which fits your healthcare needs?
Generally, there are two global types of patient portals: integrated and standalone. The former is presented as a component of electronic health records (EMR/EHR) and is fully tied to the infrastructure of a healthcare facility. Integrated portals ensure uninterrupted data exchange between doctors and patients but, in the case of ready-made solutions, are limited by the functionality offered by the specific healthcare provider.

Standalone portals, however, come in two forms: SaaS and on-premise. The former are hosted in the cloud and are available by subscription, which is especially convenient for healthcare providers within small organizations. Their advantage is quick deployment and configuration. At the same time, their customization options are often limited.
As for the second category, these are software solutions installed on local servers of a specific healthcare organization. They provide comprehensive control over data but require significant infrastructure and support costs. They can also be difficult to scale and integrate with third-party solutions.
It is worth noting that every medical organization has its own regular processes and specific business tasks distributed among different departments. In particular:
- The reception desk keeps track of patient records.
- Laboratories collect, process, and store test results.
- The finance department is responsible for payments and insurance processes.
- Doctors and medical personnel work with medical records and appointments.
All the above processes can rarely be integrated into a single system, which makes it difficult to automate them using only one off-the-shelf patient portal. Moreover, medical institutions vary greatly in specialization (including clinics, dentistry, laboratories, hospitals, etc.), and ready-made products do not always meet their needs.
If we add to this the need to comply with regional security standards for patient data, it becomes clear that out-of-the-box solutions may not be viable. This is the main reason why healthcare organizations are increasingly resorting to custom healthcare portal development.
Patient portal requirements: Key features and functionalities
Now, let's check the main functionalities and features that should be integrated into a patient portal.
User authentication and access management system
This portal component uses OAuth 2.0 and OpenID Connect for secure login. It protects users' credentials and enables multi-factor authentication. Usually, developers provide multi-level access with restrictions based on user roles (including patients, doctors, administrators, etc.).
At the same time, when implementing role-based access, it is important to adhere to widely recognized patient data security policies, such as HIPAA and GDPR. Specifically, doctors and administrators should have full access to all patient data. In contrast, individual patients should only be able to view, edit, and delete their info.
Medical data storage
The storage is located on local or cloud servers using AES-256 and TLS 1.3 for data encryption. By the way, many cloud vendors have ready-made solutions for healthcare organizations that meet the standards of patient data privacy (including AWS HealthLake, Azure Healthcare, and others). It is also crucial to ensure that such storage is protected against data misuse and unauthorized access.
Integration with EHR systems
This integration is necessary for consolidating patient data. Thus, developers must adhere to FHIR and HL7 standards to ensure compatibility and data exchange. As for the integration itself, if we are not talking about legacy solutions, it is carried out through an API.
Finally, to ensure that the patient portal system complies with the requirements of the National Coordinator for Health Information Technology (particularly, the ONC's Cures Act), it is essential that the platform could get full access to the patient, with all the ability to edit and delete.
Appointment schedules, doctors’ cards, and telemedicine tools
The first two components involve creating a catalog with therapists’ information and a scheduling system where patients can book visits. This can be achieved through RESTful API to synchronize with hospital calendars. Also, integrating with trusted video communication platforms like Zoom Healthcare can facilitate direct communication between patients and doctors.

Automation of bill calculations and online payments
Online payments are processed through integrations with payment gateways like Stripe or PayPal. In general, they must support PCI DSS standards. As for the automated billing system, this is essentially a regular calculator that “pulls up” data on the cost of services selected by the patient and sums them up (minus insurance and benefits, if any).
Integration with wearable devices
This is necessary so that doctors can monitor the condition of patients in real time. To do this, developers use APIs to collect data from devices (for example, from Apple HealthKit or Google Fit, as well as more specialized IoT equipment). At the same time, they must also implement a mechanism for obtaining prior patient consent to collect personal data.
Messaging
It also makes sense to integrate a chat (with the ability to attach media files) for interaction with doctors, supporting end-to-end encryption (E2E) and using WebSockets protocols that provide real-time messaging.
User dashboards
The patient portal needs an interface for each user role. Basically, it should adapt the data and tools for doctors, admins, and patients. Among other things, it can also be enriched with advanced analytical tools. For example, Power BI or Tableau can be used to generate reports and visualize data (assessing attendance dynamics, treatment results, patient satisfaction, etc.).
How to develop a patient portal software: From concept to launch
When it comes to custom solutions, our telehealth website development services are provided in several subsequent stages. Let’s consider them in detail.
Ideation and requirements analysis
At this stage, our team consolidates the portal concept of custom healthcare portal development, according to your business goals, unique aspects of your internal business processes and IT infrastructure, the needs of the target audience, and an analysis of competitors’ strengths and weaknesses. Based on this blueprint, we create documentation indicating functional and non-functional requirements.
Architecture design
From now on, our patient portal development team has everything ready to define the project's technological stack (for the frontend, backend, and database) and choose a specific architectural approach. We also approve the necessary third-party Integrations (including EHR, payment gateways, telemedicine solutions, etc.).
Finally, we select tools and protocols to ensure our portal has a proper security level, including data encryption, user authentication/authorization methods, diagrams of interaction between components, etc.
UI/UX design
This stage involves building interface prototypes and gradually transforming them into a full-fledged design after usability testing. At the same time, our patient portal app development experts always take into account the requirements for the accessibility of the user interface. Basically, they are most accurately outlined in the WCAG 2.1 and ADA guidelines.
Development
Now, we can start working on the frontend and backend of the patient portal. Once individual functional modules are ready, we conduct unit testing to prevent hard-to-fix bugs at later stages of the project. This stage also involves the implementation of security mechanisms and integration with third-party solutions.
Testing and quality control
When the code base is ready, our patient portal development experts conduct rigorous testing, including functional, load, security, usability, etc. This stage ensures that the solution meets the best specs and software quality standards in healthcare.

Deployment and launch
Before launching the portal, we prepare all the necessary infrastructure, build a CI/CD pipeline, and set up a monitoring system. If needed, we can train your staff on how to use the portal. After all the previous stages are checked—we usually start deployment.
Post-release support and updates
To better understand its further optimization, our patient portal development experts regularly check the portal’s logs and metrics, collecting feedback. In addition, as post-release bugs are discovered, we fix them and, if necessary, implement new features.
Understanding the needs of your patients
A patient portal and medical website design should fully adapt to the target audience's problems. That is why it is essential to define them in advance. Based on our experience, we would like to highlight the following ones:
- Long wait time when making an appointment.
Patients often encounter long wait times in phone and in-person queues. A patient portal can help. It lets users book online appointments 24/7 and choose a specialist. In addition, it sends SMS or push notifications to remind patients about upcoming visits. - Lack of full access to medical data.
Many patients are forced to visit clinics because healthcare organizations still document their test results manually. The patient portal gives access to electronic medical records, test results, and doctor recommendations, which can be easily downloaded or saved (for offline access). - Lack of understanding of the treatment plans.
Patients may find it difficult to track their treatments' progress, which may result in forgotten, delayed, or canceled visits and procedures. To prevent this, portals display the treatment plan and the current status of therapy. In addition, patients get notifications about upcoming procedures, calendars, and recommendations, which is very smart. - Difficulties in paying for medical services.
The need for patients to be physically present makes offline payments resource-intensive. Patient portals eliminate this headache with integrated payment systems, allowing users to view their payment history and current bills in just a few clicks. - Insufficient communication with the attending physician.
In-person appointments to explain test results and treatment plans can be time-consuming for both patients and healthcare providers. Patient portals streamline this process with online chat and video calling capabilities. - Weak control over the treatment of chronic conditions.
Patients with chronic conditions often lack convenient tools for regular monitoring. Portals can address this with real-time health data visualization, medication reminders, and appointment scheduling, as well as integrating with wearable devices for continuous data collection. - Low involvement in the treatment process.
Since some patients find it difficult to understand how their actions affect treatment results, the patient portal development team can also add interactive tools to the portal to track patients' treatment progress or provide educational materials.
Gamification elements can enhance the effect.

Patient portal development challenges and solutions
In this section, we will analyze the most typical challenges of patient portal software development and the most effective ways to overcome them.
- Ensuring compliance with regulations.
Telemedicine hugely relies on strong data protection, first—to comply with laws like HIPAA and GDPR, and second—obviously, it is for patient trust. End-to-end encryption, role-based access control (RBAC), and multi-factor authentication are key practices, along with regular system audits and penetration testing to ensure security. - Integration with existing solutions in the organization's IT infrastructure.
Many healthcare providers still use older systems that don't easily connect with modern software. To solve this, developers can build 'middleware'—software that acts as a bridge—to automate data transfer between patient portals and other systems, ensuring everything works smoothly. - Ensuring high performance and scalability.
Many portals frequently freeze when user traffic exceeds the original design capacity. To solve this, developers can host the portal in a cloud environment that scales as users grow and use a microservice architecture to balance the workload across the portal's services. Additionally, they can optimize a database through indexing and caching. - Ensuring intuitiveness.
Since the target audience of patient portals is diverse (including the elderly, people with disabilities, and people with no technical literacy), there should be universal access to the full use of all portal functionality. To solve this, during the development of the patient portal software, the team should conduct user research and surveys to guide and optimize the software effectively. They should also adhere to the compliance of this software with the WCAG 2.1 guidelines.
- Accessibility on mobile OSes.
As patients increasingly manage their healthcare on digital devices, patient portals must offer a seamless mobile experience. Poor mobile optimization can lead to slow loading times and display issues. Developers can address this by building progressive web apps (PWAs) or cross-platform solutions, implementing offline access for key features, and optimizing content loading with techniques like lazy loading and data compression.
Patient portal software cost: What to expect
The cost of telemedicine app development depends on project complexity, the team involved in the patient portal software development process, geographic location, development timeline, and the scope of features. Let's examine each of the points that influenced the cost in detail:
1. Project complexity
- Basic consultation apps with user registration, appointment scheduling, video calls, and messaging: $30K-$100K.
- Advanced telehealth platforms with multi-user portals, integrated EHR, and health analytics: $100K-$300K+.
- Telemedicine platforms with IoT/AI integration: $250K-$500K.
2. Team composition
A typical team for creating a basic patient portal usually includes:
- 2-3 developers: Where 1-2 are front-end developers, and 1 back-end developer.
- The project manager: Tracks the project goals and wins.
- QA specialist: Tests the app to make sure it works correctly.
3. Development timeline
The time it takes for patient portal software development also affects costs. Most telemedicine apps take between 2 to 6 months to develop:
- Simple apps usually take about 2-3 months.
- More complex apps may take up to 6-12 months.
4. Geographic location
American tech experts can be expensive. For example, a front-end developer might earn over $100K annually, about $8K monthly. He might charge between $70K-$80K for a three-month project.
Hiring remote developers can save you money. For instance, Eastern European developers or other regions often charge between $2,500 and $3,500 monthly. You can easily hire a similar team for about $30K to $40K for the same project.
If you want to find out the patient portal software cost in your case, please fill out this contact form.
Improving patient outcomes with data management: A case by Darly Solutions
From theory to practice—let's examine our relevant Darly Solutions experience through a top case from our portfolio.
In particular, we were approached by a HealthTech company specializing in consolidating unstructured medical data for organizations in the healthcare sector. They needed a custom digital solution to monitor clinical data.
Faced with a tight deadline and the need for high precision, we meticulously planned and assigned all the UX/UI design, web development, QA, and project management tasks. We also reviewed the team's work schedule, as some members had to work overtime. Finally, we carefully chose the technology stack. We settled on Angular, HTML, CSS, Docker, ngRx, TailwindCSS, NGX Pagination, and JSON.
Finally, our efforts paid off. We launched the product on time and met all design, functionality, and quality standards. As a result, the client has a competitive product with all the chances to thrive in the innovative telemedicine sector.
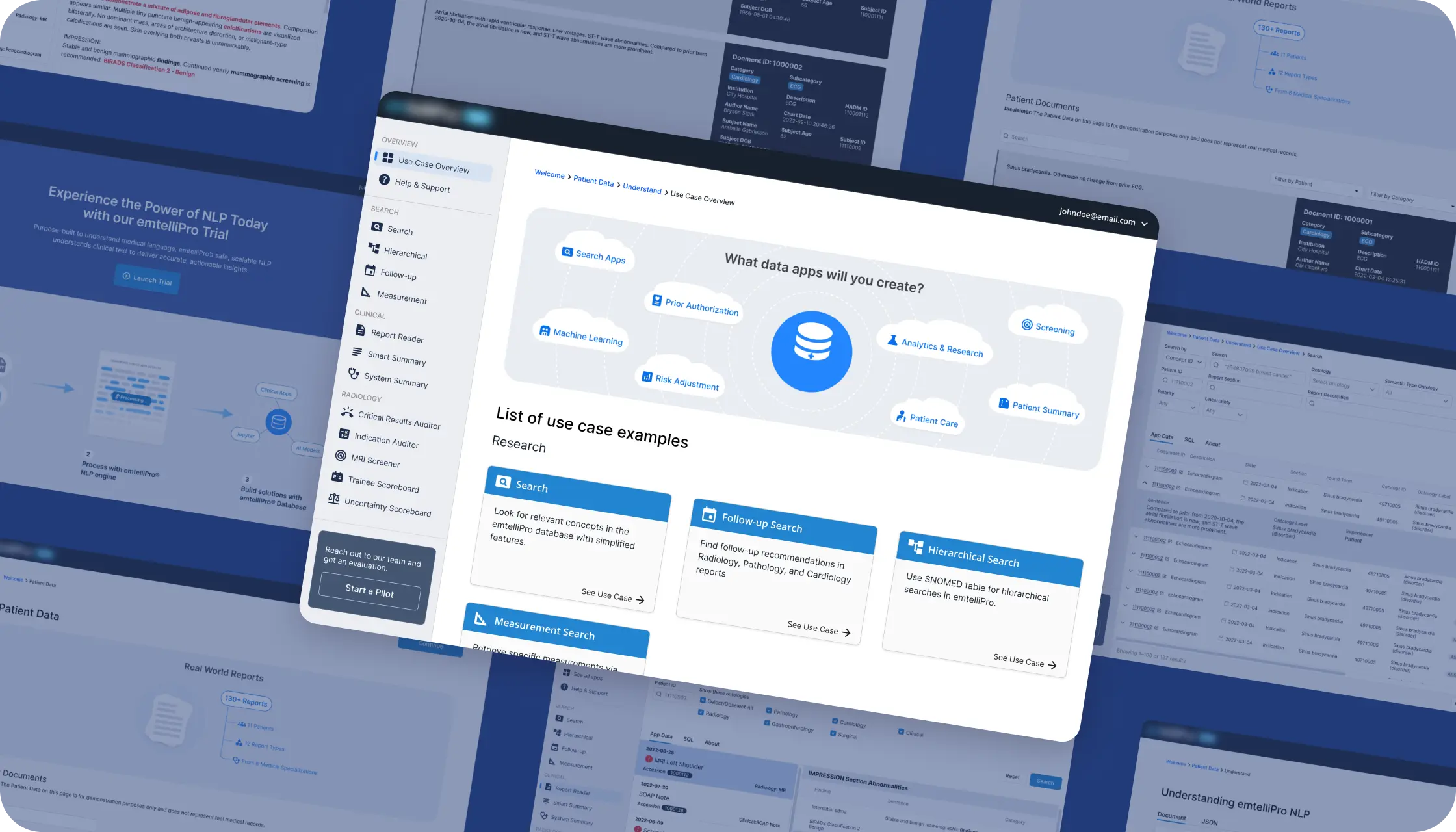
Find out more about this case here.
The future of patient portal development
In general, the future of patient portal software development is closely connected with the fast development of modern technologies, such as:
- Artificial intelligence and machine learning.
These technologies will personalize the portal and related healthcare services. AI-powered chatbots, including ones with recognition of human voice commands, will assist with scheduling appointments and answering FAQs. In advance, machine learning can also analyze patient data and symptoms to provide preliminary diagnoses.
- Blockchain.
The introduction of blockchain technologies in patient portals can be aimed at more secure storage of their medical records and ensuring access to them only to authorized users. In addition, with its help, each interaction with data (adding, editing, and deleting) will be recorded, increasing the system's transparency.
- Virtual and augmented reality.
These technologies can form the basis of next-generation telemedicine solutions. In particular, in the future, patients will be able to interact with doctors at a distance without reducing the quality of service. AR interfaces will also help inform patients about upcoming treatment plans.
- Internet of Things and integration with wearable devices.
IoT solutions can provide end-to-end RPM in real-time (for example, portals will be able to collect and analyze data on the patient's pulse, blood pressure, oxygen level, and activity). Based on this data, doctors can receive instant notifications of critical changes regardless of patients' locations.
- Big data and business intelligence.
Examples of patient portals use big data to identify trends, such as tracking the rise in the incidence of a particular virus or assessing the effectiveness of treatments. Also, end-to-end medical data analysis ensures timely prediction of exacerbation of chronic diseases. Finally, doctors and administrators of healthcare institutions will be able to monitor departments' workloads and optimize appointment scheduling.
- Biometric identification.
Biometric mechanisms can give users access to the portal through fingerprint, face, or voice scanning, making the authorization process more secure and easier.
Conclusion
Now you know everything about patient portal development and can safely choose an off-the-shelf solution or search for a team to implement a custom one. If the second option is closer to you but you would not like to turn the search process into a real headache, you can contact us, and we will be happy to discuss the details of our future cooperation to implement your idea.


In 2024 alone, the medical imaging software market size reached $8.11B. By 2029, it is projected to grow to $11.83B and up to 7.84% at a CAGR. This is a fairly predictable trend due to the development of AI. Especially since big data, cloud technologies, and other advancements are already significantly speeding up the accuracy of diagnostics.
If you are considering custom development of medical image analysis software, now is the most favorable time. Below, we will reveal the specifics of creating such solutions and describe the requirements and the challenges you may face.
What is the definition of medical imaging software?
Medical imaging software—it's the digital tool doctors use to examine medical images. Think X-rays, MRI and CT scans, ultrasounds, PET, and other radiology scans. Basically, it helps to see the details of every complex illness and make informed decisions about patient care.
To maximize efficiency, medical imaging software integrates a range of advanced technologies. These include AI for anomaly detection, ML for image segmentation, and methods for filtering, contrast enhancement, and noise reduction to improve image quality.
Also, 3D reconstruction technologies create volumetric models of organs and tissues. Developers also rely on the DICOM standard for medical images as it allows seamless transfer. They also use cloud tech to access data, integrated medical records, and VR and AR to visualize data and create interactive interfaces.
As a result, with medical image analysis software, healthcare organizations reduce the workload of their doctors and researchers and minimize the likelihood of misdiagnosis.
Examples of medical imaging software
To better grasp how these solutions work, we suggest you look at several medical imaging software examples that have gained worldwide recognition.
RadiAnt DICOM viewer
It is a high-performance medical imaging software that processes DICOM images. Due to its rich functionality, both doctors and researchers use it in their work. It has smart multimodality tools for 3D and 2D visualization and MPR (multiplanar reconstruction). Moreover, developers made the interface very user-friendly, so this software is also a great choice for users with low technical skills.

OsiriX MD
Specifically designed for macOS, OsiriX MD is a powerful DICOM platform that meets the needs of radiologists. Its advanced capabilities support 3D and 4D image analysis, hybrid imaging with PET-CT and PET-MRI, and integration with PACS servers. Crucially, it is FDA- and CE-certified for clinical us.

Horos
Horos is a free OsiriX-based DICOM viewer available on macOS. It has rich customization options for analyzing volumetric data, such as 3D reconstruction, and is especially useful for students and researchers.

GE Healthcare Centricity PACS
GE Healthcare Centricity PACS is a proprietary enterprise medical image analysis software. It has EHR and EMR integration, real-time collaboration, advanced AI analysis, DICOM standards, and format support. It can be a full-fledged assistant for doctors and researchers.

Philips IntelliSpace Portal
Tailored for large clinical institutions, Philips IntelliSpace Portal excels in medical image analysis and visualization. It integrates AI-driven automation and tools for multiparametric imaging in cardiology, neurology, and oncology; this medical imaging software supports multi-user collaboration.

Key features of medical image processing software
This section explores the key functionalities typically found in standard medical imaging software.
Tools for viewing and processing medical images
Ensure your medical imaging software works with various input data (CT scans, MRI scans, X-rays, ultrasounds, and hybrid studies like PET-CT and PET-MRI). Usually, this is done by supporting the DICOM format. In addition, you will need tools to scale, rotate, and adjust image contrast. So, optionally, develop a panel for 3D and 4D visualization, including multiplanar reconstruction.
AI-driven image analysis
AI is key in automating the detection of anomalies in medical scans. It can identify cancerous tumors, blood clots, and fractures early, with a high degree of independence. Also, AI in your medical imaging software can classify pathologies using trained models. It can segment organs and tissues on scans and analyze multiparametric data.
Diagnostic and treatment planning tools
This includes tools for creating 3D models, surgical planning, and evaluating the effectiveness of treatment. You should also consider integrating your medical imaging software with robotic surgical systems.
Medical data management tools
To implement effective medical data management, you will probably need to integrate your medical imaging software with PACS (for storing and transmitting data), EHRs (for centralized access to personal patient information), and cloud solutions (for unimpeded access to images from anywhere in the world where there is an Internet connection).
Collaboration tools
It's mainly for remote access so doctors and specialists can chat and comment on each other's actions. It also involves integrating telemedicine platforms to discuss complex cases and hold educational seminars.
What development?

A wide range of organizations can benefit from medical image analysis software development. Now, let's find out which areas of healthcare benefit from medical imaging software the most.
- Cardiology.
In this field, medical imaging software is mostly used to analyze CT and MRI of the heart and angiography. In addition, it monitors treatment effectiveness, plans operations, and predicts cardiovascular disease risks.
- Dentistry.
Inevitable for 3D scanning when planning dental implants, diagnosing jaw diseases, visualizing root canals, etc.
- Oncology.
Here, medical imaging software detects and classifies tumors, tracks their growth, and assesses treatment effectiveness.
- Neurology.
In this sector, medical image analysis software analyzes brain MRIs and CTs and provides 3D visualizations to assess the spine and nerves.
- Orthopedics.
Orthopedics studies thrive on precise X-ray analysis, which includes 3D joint modeling and spinal disease diagnostics.
- Mammology.
Medical imaging software can detect microcalcifications and early breast cancer through comparative analysis of changes in mammary gland tissue.
- Urology.
In this industry, medical imaging software helps diagnose kidney and bladder diseases. It does this by analyzing CT and ultrasound images. Additionally, the software can help plan operations and monitor patients with chronic diseases.
- Pulmonology.
Industry specialists can use such software to diagnose lung diseases, analyze chest CT data, and assess COVID-19 damage.
- Gynecology.
In most cases, medical image analysis software is used to perform pregnancy ultrasounds. It helps monitor the fetus, find pelvic tumors, and analyze the endometrium and other tissues.
- Traumatology and emergency medicine.
In traumatology, 3D medical imaging software can quickly diagnose fractures and internal injuries. It can also visualize organs for urgent decisions.
Still, deciding on the right healthcare sector for your medical imaging project? Contact us and discuss the possibilities of its practical implementation with Darly Solutions' experienced developers.
Medical imaging software development: Steps to follow
Custom development must follow clearly defined stages that most teams use. But, it can still be approached in various ways. Below, we outline how healthcare software development services are delivered in our company.

Concept formation
Start your medical imaging software project with market analysis. Define the target audience, prioritize tasks the software should solve, and research competitors (to identify their strengths and weaknesses). Based on the insights, our medical imaging software development team assesses the functional requirements and evaluates the need for specific technologies to handle image processing. This ensures that the chosen solutions align with the project's technical needs and optimize the processing of healthcare-related images.
Planning
Once we agree on the conditions with all stakeholders, we will write a technical specification for your medical imaging software. This document will describe its functionality, interface, API, security, and integration requirements. We will also approve the tech stack and necessary integrations. Finally, we create a roadmap that defines the milestones and deliverables for each medical imaging software development project stage.
Prototyping
Now that everything is ready, we can begin creating user stories. They include handling DICOM file uploads and 3D models, among other key tasks. For UX/UI best practices of safe data, we follow the WCAG 2.1 guidelines. They ensure accessibility for users with varying technical skills. We also test prototypes with focus groups to see feedback on complex features, which is helpful for future design improvement. Finally, after the edits are done, we develop a full-fledged design.
Coding
The frontend has algorithms to process and analyze medical images. The backend ensures secure data transfer between the medical imaging software and storage. It also encrypts data and protects against vulnerabilities like SQL injections. These involve writing database queries for smooth software interactions and data storage interactions. And last but not least—we also integrate with your healthcare org's existing systems and services (if any).
Testing
Once the code for your medical imaging software is ready and all components have passed unit tests, we run complete test cases. We check for load, functional, non-functional, security, and usability issues.
Deployment
At this stage, we are choosing hosting for your medical imaging software (usually either cloud or local servers), setting up CI/CD, and training end users, for example, by providing them with documentation, training materials, or live courses. Once we've done it, we deploy the solution (first in the test environment and then—in the actual usage environment).
Support and updates
Finally, after the medical imaging software is deployed, we set up monitoring systems to track its performance and detect errors, fix post-release bugs, optimize it according to user feedback, and add new features if required.
Key tech specifications for medical imaging software development
Such software development can be complex, especially in its early stages. Basically, there is often no clear way to turn an abstract idea into actual requirements.
So, let's examine all the key tech specifications that are usually implemented in medical imaging software apps:
- Support for common medical image formats such as DICOM (including DICOM tags for metadata) and standards for storing, transmitting, and processing medical images (such as C-STORE, C-FIND, and C-MOVE).
- Compatibility with various devices (CT, MRI, ultrasound, etc.).
- Image processing can improve images by adjusting contrast brightness and applying filters. It can also segment them to highlight organs and tissues. Lastly, it can register them to compare scans over time.
- 2D and 3D visualization, including volume rendering (CT/MRI), support for iso-sections and reconstructions, and interactivity (e.g., rotation, zoom, and pan).
- Data security, including HIPAA and GDPR compliance, support for TLS (for data transfer) and AES-256 (for image and metadata storage) encryption standards, as well as access control with role-based authorization and two-factor authentication.
- PACS and EHR/EMR integration (e.g., via HL7/FHIR).
- Annotation (adding labels, arrows, and text comments) and providing real-time collaboration tools.
- PDF report generation and image export.
- Scalability (including horizontal scaling via the cloud), multi-threading, and hardware acceleration.
- WCAG 2.1 compliance and user interface customization.
- Logging and monitoring events (including loading, processing, and exporting scans), auditing user access, tracking system performance, and setting up failure notifications.
- Local deployment of software on physical servers (most likely, this will require ensuring compatibility with Linux and Windows OS).
- Setting up regular data backups and automatic recovery after system failures.
Of course, this is just a basic list of specifications. In practice, your project team will expand and refine the list of features while specifying the tools and technologies for the project's unique needs.
Medical imaging software development cost
When it comes to the development cost of medical image analysis software it depends on its complexity and the technologies used. Without data and business needs—it's hard to define the precise price, but on average, basic DICOM (Digital Imaging and Communications in Medicine) typically ranges from $30K to $300K. A customized version of Basic DICOM may cost $30K to $50K. Advanced customizations could cost $70K to $150K.
Implementation costs differ based on the size of the practice:
- Small practices typically cost $5K to $10K and take 1 to 2 weeks.
- Medium facilities cost $20K to $50K and take 1 to 3 months.
- Large enterprises may cost $100K to $200K and take 3 to 6 months.
Please complete this form to calculate the precise budget for your medical imaging software development idea. We will contact you shortly.
Challenges in medical imaging software development
Let's examine the main challenges encountered when developing medical imaging software.
- Regulatory compliance.
Software handling sensitive data, like patient information, must comply with HIPAA, GDPR, FDA 21 CFR Part 11, and CE Marking regulations. Key security measures include code audits, RBAC, 2FA, and strong encryption (e.g., AES-256, TLS).
To avoid fines, consult a local lawyer on medical standards.
- Integration with existing systems.
Integrating PACS, EHRs, and other systems requires DICOM, HL7, and FHIR support. Also, medical organizations have very different established IT infrastructures, which makes it hard to unify their software. If you create a universal solution, you must provide some middleware. It will help users adapt to various services and systems.
- High performance and scalability.
Medical images, especially CT and MRI, are large. This can slow their processing and increase resource needs.
In this regard, you may need to implement lossless compression mechanisms for images and multithreading and parallel data processing algorithms. By the way, a common fix is to move your software to a cloud solution designed for healthcare businesses.
- The complexity of big data management.
Storing and processing massive data, like images and metadata, require a careful choice of databases and storage. In particular, this implies a preference for distributed databases and object storage.
For even greater reliability, do not forget to provide backup and auto-recovery.
- Risks associated with cyber attacks.
Cyber attacks that leak medical data are a serious problem for healthcare software. To solve it, you must implement constant monitoring. Also, set up regular security updates, including patches and OS updates.
Finally, train your staff on social engineering. It can reduce the risks of phishing attacks.
Providing a user-friendly interface.
Interfaces for doctors and medical personnel should be user-friendly and intuitive, requiring minimal technical training to operate efficiently. To achieve this goal, you must test hi-fi prototypes on the real target audience and perform subsequent optimizations. Also, do not forget to ensure your interface is created under the WCAG 2.1 guidelines.
The future of medical imaging software
Medical imaging software development will advance by adopting the newest technologies, process optimization, and increased integration with other medical systems.
So, here are the core areas in which medical imaging software can be optimized:
- Speeding up diagnostic.
- Increasing image recognition accuracy.
- Costs reduction.
- Improving user experience.
This can be achieved through the implementation and development of the following technologies:
- Artificial intelligence and machine learning.
For highly accurate and automatic analysis of medical images and accelerated diagnostics.
- Cloud computing.
To provide quick access to medical images from anywhere in the world, process large amounts of data without the need to upgrade local infrastructure, and implement remote collaboration between healthcare specialists.
- VR/AR.
Medical imaging software development allows anatomy and pathologies to be studied using interactive 3D models and visualize the patient's anatomy before surgery.
- Quantum computing.
While most quantum computers are not yet available for widespread use, they will speed up processing large datasets and training neural networks for image recognition in a few years.
- Blockchain.
To guarantee the immutability and protection of data from medical imaging software while providing patients with comprehensive control over their medical information.
Our experience in medical imaging software development
This section covers the development of the PrismaORM brain scanner. This platform was crafted for chiropractors, neurologists, and neurosurgeons to monitor brain activity and brainwaves before, during, and after chiropractic treatments.
First, we assembled a team of eight experts to bring this vision to life. They worked closely with two external teams of medical imaging software engineers. We've pointed out a tech stack based on PostgreSQL, Typescript, React Native, Nest.js, Expo, Three.js, and SQLite. This tech of choice lets us build a platform that processes real-time data from brain activity helmets. The BLE protocol transmits this data. A tablet interface visualizes it. A key to the project's success was optimizing the user experience. This included better platform performance and integrating 3D models.

As a result—we've made a powerful tool that empowers medical professionals to conduct more precise diagnostics and offer more effective treatment recommendations.
For a detailed look at this project, visit our portfolio.
Wrapping up
Now that you understand the specifics of medical image analysis software development, you can begin searching for a team to bring your project to life. We are a reliable provider of custom healthtech solutions, ensuring a smooth, transparent, and predictable collaboration. Simply fill out the form, and we'll get in touch as soon as possible to discuss your medical imaging software project in detail.


From long patient wait times to inefficient manual processes and risky paper records, the healthcare sector has faced numerous challenges historically. This has created a fertile ground for doctor appointment apps. According to Verified Market Reports, in 2023 alone, the market was valued at an estimated $318.49M, projecting a surge to $862.16 million by 2030 (15.29% CAGR).
Given the growth of AI-based solutions in telemedicine tech and the modernization of the healthcare system, we can now highlight the importance of such solutions and dive deep into the specifics of healthcare appointment apps.
What is a doctor appointment system?
A doctor appointment application — is a digital solution that automates the registration of patients for an appointment with medical specialists. However, modern solutions imply more than just scheduling online appointments. They give patients useful information about a healthcare institution's services and specialists. Also, they connect patients with doctors and give access to their records in the comfort of their homes.

Why is this system gaining traction in the healthcare sector? Let’s break it down into factors:
- The widespread digitalization of the healthcare sector.
Healthcare is moving beyond in-person consultations in the facility. Now, it includes remote consultations, app-based therapies, and remote health tracking for timely interventions. - The development of modern technologies.
Various mobile applications and the affordability of smartphones make this format of interaction with patients desired and preferable. - Reducing the workload on administrators.
To prevent personnel burnout, medical institutions can use healthcare scheduling software systems to reduce the number of routine tasks assigned to administrators and the number of errors associated with the human factor. - Increased patient satisfaction.
Transparent access to doctors' schedules and the ability to choose a suitable time — increase customer loyalty. - Increased occupancy of doctors' schedules.
With a doctor appointment system, healthcare organizations can minimize empty appointment slots since it will be easier for patients to choose the optimal date and time for a visit.
Key doctor appointment app features
Since the Apple App Store boasts approximately 35,019 healthcare and medical apps, among which are approximately 10 to 20 types of doctor appointment apps, features might hugely range from app to app. Let's examine the main features of the doctor appointment app.
Online appointment booking
The system should have filters for doctors by specialization, review patient feedback, and book appointment availability by date and time. Additionally, patients should be able to receive reminders for upcoming appointments (e.g., push notifications, email, or SMS).
Telemedicine
For routine follow-ups, an online medical appointment system is essential. It's not a choice but an inevitability. Both patients and healthcare providers save travel time and can schedule appointments just in the app via online consultations, video conferencing, or text chat.
Integration with EMR and billing system
Integration with electronic health records provides access to the patient's medical data directly from the application, allowing doctors to update and review these records directly from the platform. As for the billing system, the PCI DSS-compliant payment gateway will be the core element of the online payment process. In addition, it provides an option for generating bills and receipts.
Feedback and ratings
Usually, this is a window where patients can rate their experiences and write reviews for specific providers using a simple scoring system. For usability, this feature must remain unobtrusive within the app interface.

FAQ and educational materials sections
The app should include a FAQ section covering usage and privacy. It should also have an educational section with information about specialists, a map of the institution, and service costs.
Monetization strategies for doctor appointment apps
The ideal monetization strategy for a doctor appointment system depends on the target audience and the organization's business model. Let's look at the most popular types of monetization in this niche:
- Subscription-based.
According to this model, after paying for a monthly or annual subscription, patients get access to advanced features, such as priority appointments or online consultations. - Pay-per-booking.
This model involves charging a fixed fee or a percentage of the service's cost (usually 5-10%) for each appointment. - Advertising.
Based on this model, you can publish advertisements for medical services, pharmacies, insurance companies, and other partner organizations. This can be contextual advertising, static banners, or affiliate programs (for example, you can recommend pharmacies for buying drugs). - Payments for telemedicine services.
This approach to monetization involves charging a fee (either a percentage of the service cost or a fixed amount) for online consultations implemented within the application. - Patient data monetization.
This type of monetization involves selling anonymized patient data to global healthcare corporations. They can be used in the future for both clinical research and to improve the quality of services of partner organizations (for example, insurance companies, laboratories, etc.). - White-label solution.
Finally, you can develop a customizable solution and sell it to other companies under their brand. In this case, you must provide a settings panel where each organization can set individual configurations.
Benefits of doctor appointment booking app development
To understand the benefits of the doctor appointment booking system, we first need to figure out the main pain points such software can solve. Previously, we’ve mentioned some, but for the sake of completeness, let's consider each of them:
- Simplification of the procedure for making an appointment with a doctor.
Earlier, patients had to call the clinic, wait for the admin to answer, and adjust to the schedule. With the app, they can choose the best time and date within a few moments on their smartphone. - Drop in missed sessions and treatment gaps.
With appointment alerts or medication reminders, patients won’t forget about upcoming visits to the doctor and taking medications, which ultimately saves the clinic's resources.
- Transparency of pricing.
Some patients find it difficult to understand the cost of the services; in turn, with the application, they will have access to all the price information before making an appointment. - Comprehensive information about doctors and services.
To prevent patients from choosing doctors blindly, the application can offer them a convenient rating system, reviews, and descriptions of services; thanks to this, they will make a more conscious decision about choosing a particular doctor/service.
- Minimization of paperwork.
Without a doctor appointment application at hand, medical personnel often had to work with paper journals. An app that integrates with the CRM, EHR, and other software will reduce reliance on paper docs. - Higher revenue.
You can sell additional services through the application; moreover, its convenience and transparency increase the likelihood of repeat visits. - Reduced need for human resources.
The application’s launch will help reduce the need for a large administrative staff, allowing existing employees to focus less on routine tasks and more on value-driven activities. - Greater return on marketing efforts.
The patient's behavior analytics can help you craft more targeted offers. With insights into patient habits and preferences, you can create highly targeted offers that resonate with your audience, optimizing both campaign success and budget efficiency while increasing engagement and retention. - Increased competitive advantage.
Modern clinics that offer convenient digital solutions win more patients, improve operational efficiency, reduce no-show rates, and enhance patient satisfaction, all of which contribute to a stronger competitive position in the overall healthcare market.
Steps to build a doctor appointment app
Let’s check the steps included in the medical software development services that our doctor appointment app development company provides.
Market research
At this stage, our doctor appointment app development team defines the application's target audience (the patients' age, smartphone proficiency level, etc.). Next, we analyze the institution's business model for which it’s being created while researching competitors and identifying their strengths and weaknesse

Based on the insights received, we determine the app's basic and advanced features. For example, we want real-time patient monitoring through wearables. We also need to agree on the OS, which can be Android and/or iOS. Lastly, we must choose the best monetization model. Finally, we determine the necessary integrations with third-party solutions and the requirements that must be met (usually GDPR, HIPAA, etc.).
Prototyping and UX/UI design
At this point, our experts create user stories to guide the development of prototypes (first lo-fi, and when agreed upon with all stakeholders, hi-fi). Once the prototypes are finalized, our team starts working on the full-fledged doctor appointment app design. We aim to create user-friendly navigation that cuts off the input needed from the user to complete tasks. At the same time, the team works on the UI, optimizing it for mobile platforms and obtaining WCAG 2.1 accessibility guidelines.
Architecture development
This stage involves choosing an architectural approach (for example, microservices for better scalability, REST or GraphQL for API, and so on). It is also important to plan the processes that will be implemented on the server side (in particular, record management, authorization, etc.). On the client side (usually, this is the patient and administrator interface) and on the database side (as a rule, flows for transactions and caching are separated). We also select specific solutions for implementing the necessary integrations.
Coding
Now, we have everything ready to define the technology stack for the backend and frontend. This decision is based on whether native or cross-platform development will be utilized for the doctor appointment app. Once individual program modules are ready, we proceed with coding and testing each component.
Testing
Since the entire code base is ready, our doctor scheduling app development team ensures that it is fully covered with test cases to perform integration, load, and other types of testing. If there are any bugs, we will fix them immediately and then test the product again. Repeat this process until we meet all the specifications.
Launch and deployment
Finally, our doctor app development experts set up the server infrastructure (optionally, they also introduce CI/CD practices). Ensures data security (through encryption and regular security audits) and carries out a test launch of the software. If there are no critical bugs in the beta version of the application, we release it in the App Store and/or Google Play.
Post-release support and development of updates
This stage includes maintaining app stability, fixing failures, adding new features, optimizing existing ones, updating the design, and scaling with the growing user base.
Doctor appointment app design: Best practices
When it comes to the UI design of a doctor appointment app, we prioritize WCAG 2.1 guidelines. This section details and provides practical examples of their effective implementation for an optimal user experience.

- Readability of information.
Maintain a color contrast ratio between text and background (at least 4.5:1 for normal text and 3:1 for large text). Also, include doctor avatars and icons, ensure text scalability up to 200% (without loss of functionality), and add subtitles and text transcripts for videos (if any). - Ease of navigation.
All UI elements should be keyboard-accessible and have a minimum clickable size of 44x44 pixels. Ensure there’s extra space around buttons or links to prevent accidental clicks and include breadcrumbs for easier navigation. - Clarity of the interface.
Use simple language in the interface, label all form fields, provide input format examples (like "dd.mm.yyyy"), highlight errors, and offer step-by-step instructions for complex tasks, including a progress indicator. - Interface reliability.
Ensure that your application is compatible with assistive technologies (for all functional elements, use ARIA labels). Test your app on various devices and ensure it uses standardized data formats like JSON and XML for smooth communication with integrated third-party servic
Of course, this is only a small part of the best practices you can implement in the doctor consultation app development process. To maximize the loyalty of your audience and better understand what the design should be — read the WCAG 2.1 guidelines directly.
Doctor scheduling app development: Overcoming key challenges
Generally speaking, everyone who is going to develop a doctor appointment app faces challenges to one degree or another. To overcome them effectively, it's crucial to understand them in advance. Let's explore them in detail:
- Integration with software solutions that you already use.
Your application may require integration with systems and services that are either legacy or support non-standard data exchange protocols (i.e., different from HL7 and FHIR). In this case, you may need additional middleware development to ensure seamless data transfer. - Data security.
Medical information must be protected with particular care, as its leakage can lead to large fines and loss of reputation for your organization. To minimize risks, consider data encryption at rest and in transit, implement two-factor authentication and role-based access control. After all, try to regularly conduct pen-tests. - Performance and scalability.
High server load during peak hours can lead to failures in the operation of your application. To prevent this, you can initially choose cloud platforms that support autoscaling for hosting and implement data caching. - Testing complex scenarios.
During testing, your QA specialists risk missing complex interaction scenarios with the application. For example, when several patients simultaneously make an appointment for the same doctor or when the selected order of visits to several doctors is conflicting. To ensure comprehensive coverage of test cases, use automated testing tools. - Accessibility.
A confusing interface can drive users away, leading to fewer interactions with your app. To prevent this, conduct thorough UX research with real users before launch. Based on their feedback, make necessary adjustments to the app's functionality and design. - The unwillingness of personnel to switch to new digital solutions.
Adjusting to new rules might be hard, especially within historically established healthcare practices. You might consider providing training for your staff on how to manage new progressive software.
Beyond technical challenges, there are many business-related obstacles, from USP's definition to the choice of an effective monetization model. This is why, besides carefully selecting the right doctor appointment app development team, consider hiring skilled marketing experts, too.
Doctor appointment app development cost
From our experience of doctor appointment mobile app development, it is impossible to determine the accurate cost of such a project without understanding its functionality and the platforms it is intended for. However, based on the average cost for app development, we can give an approximate cost guide. Here’s a breakdown:
Complexity of projects:
- Simple apps typically range from $20K – $30K, and their implementation takes 4 – 6 months. These apps usually include basic functionalities like appointment scheduling and doctor search features.
- For medium apps like telemedicine integration and electronic health records (EHR), costs can rise from $30K to $45K with an approximate 6 – 9 months timeline. This includes both web and mobile platforms with a broader range of functionalities.
- Highly complex applications with real-time video consultations, comprehensive analytics dashboards, and AI-driven functionalities may exceed $45K+ and take 9 – 12 months.
Geographical variations
The cost can also vary by region:
- North America: Because of advanced technological capabilities, on average, it has the highest cost, ranging from $30K – $150K+.
- Europe: Cost ranges from $20K – $150K, influenced by economic conditions from country to country.
- Asia: Development costs are generally lower, ranging from $20K – $100K.
Have a thriving idea for a doctor appointment app and are curious about a budget estimate for its deployment? Simply fill out this form, and we will swiftly calculate your project and contact you back.
Top 5 successful doctor appointment apps
Now, let’s explore some top-tier doctor appointment apps that excel in every aspect. These examples might inspire you to build a doctor appointment app for your healthcare organization.
Zocdoc
Zocdoc is praised for its intuitive interface and powerful search tools. The platform has an intuitive interface and powerful search tools. The platform streamlines appointments and has instant confirmation features, reminders, a feedback system, and seamless integration with insurance providers and document uploads.

Practo
Popular in India, Practo gives patients access to doctor appointments, telemedicine services, ordering medicines for delivery, and storing medical records. Patients can view individual doctor profiles, including their education, experience, and certifications, allowing them to choose the best specialists for their treatment.

Doctolib
The Doctolib application simplifies making appointments with doctors and provides the option to cancel a visit. This application is integrated with doctors' calendars, automatically sends notifications, and provides rich functionality for doctors (including scheduling management and provision of telemedicine services).

Healthgrades
As for alternatives for the US market, we cannot help but mention Healthgrades. This application helps users find doctors and medical institutions based on location, specialization, and rating. Plus, it allows patients to make appointments and get detailed information about particular specialists and organizations.

MyChart
MyChart — is a top charted app in the US and Canada. Designed to manage medical information and schedule appointments, it allows patients to communicate with doctors online and get family access.

Darly Solutions' expertise in online booking and enhanced customer engagement
The most relevant case for online doctor scheduling app development was Glamezy, a B2C solution for the beauty industry. Our client sought to create an online platform to help small and medium businesses in the beauty sector expand their reach, especially after the restrictions imposed by the COVID-19 pandemic.
The goal was to develop a website that allowed customers to book beauty services online based on location easily. Also, the platform must have an easy and encouraging interface to communicate with potential partners while boosting sales and driving customer engagement. Ten experts worked on this project; and for the tech stack, we used React and Node.js.
As a result, we created a solution for easily searching and booking top beauty professionals. Now, the platform lets users add salons to a shortlist with one click, view nearby salons on an interactive map, and earn points for every transaction on the platform.

If you’d like to explore this case further, please visit our portfolio.
Final thoughts
It’s fair to say that at the heart of every design lies a larger goal for the benefit of humanity. A well-designed doctor appointment app boosts access and patient satisfaction while helping small and medium healthcare organizations and businesses thrive in the tech sector.
After you’ve read all the details about ideas and challenges for developing a doctor appointment app, it's time to find the right team to turn your vision into reality.
For now, don’t settle for less. Darly Solution is here to help! Contact us today to discuss your project in detail.


Specifically, according to the Exploding Topics resource, in 2024, Android has a 70.93% global market share while iOS only has about 25% of it. However, both platforms are undoubtedly popular, and each of them, with the right approach to development and promotion, can provide product owners with a stable income. Below, we will reveal the differences and similarities between iOS and Android development, paying special attention to security and customization options.
Android vs. iOS App Development: Key Differences
Let's first look at the fundamental differences in Android and iOS development.
Programming languages
When it comes to native development, the most popular Android development language can be considered Java or Kotlin (they are both officially supported by Android’s original IDE, but the last one is preferable for new projects). As for native development for iOS, here, developers will need knowledge of Objective-C or Swift (generally speaking, this is the best option for new projects, while Objective-C is mainly used to support existing solutions that were originally written in this language).
Development environment
As the primary development environment for the Android platform, Android developers use the open-source Android Studio IDE, although in some cases their choice may also fall on Visual Studio, Eclipse, and some other development environments. At the same time, iOS developers usually resort to the help of Xcode with the integrated iOS SDK.
Differences in design
iOS development requires following the platform’s own principles for user interface design listed in the Human Interface Design Guidelines (the main aspects of which are color variety without shadows (Flat Design Depth), minimalism (Clarity), and content-first approach (Deference)). In the case of Android development, these are the recommendations for recreating Material Design (the main aspects of which are expressing the hierarchy of elements through their size, colors, and shadows (Metaphoric Nature), using bold typography to highlight important elements (Bold Graphical Design), visualizing reactions to user actions (Meaningful Animation), as well as adapting the design to devices of different form factors (Adaptive Design)). Also note that Android allows the development of applications for operation in Kiosk Mode – this will be useful for businesses presenting their services and/or products through software installed on corporate Android-based devices.
Hourly rates
According to Glassdoor, the average annual salary of an Android developer in the US ranges from $91K to $135K, while for an iOS developer this range is from $101K to $174K. From this, we can conclude that, on average, the iOS app development cost (if you stick to the hourly rate for specialists) will be somewhat higher compared to the Android app development cost, all other things being equal (in particular, the same number of supported device formats and OS versions).
Complexity of development
It is worth noting that native Android development tools and iOS mobile app development tools are quite easy to deal with and, in general, have a low entry threshold. That is why the complexity of implementing software for a particular platform should be considered primarily from the point of view of ensuring compatibility. The fact is that if you are planning Android development to cover as many user devices with different form factors as possible, your team will have to spend a lot of effort and time. Also, there is the need to provide compatibility with earlier versions of Android and, accordingly, adapt the software for devices that support them. Therefore, the development process for Android can be much longer than in the case of iOS, a platform that is characterized by a relatively small number of compatible user devices. On the other hand, for iOS development, the entire team must be equipped with macOS-based devices — only then will they be able to build the software and successfully test it in an emulator.
iOS vs. Android: Security and Privacy
The main difference between iOS and Android in terms of security lies in the fact that iOS security is more focused on providing strong software protection (which is facilitated by its closed nature and limited number of supported devices), while Android focuses on a combination of software and hardware protection (due to its initial open source nature, which can still be violated by individual vendors creating their own Android-based OSes, as well the variety of supported user devices). In the end, it is impossible to say that one of these operating systems is more secure or, on the contrary, more vulnerable, since by following the standards and generally accepted rules of secure development, you will be able to achieve optimal compliance for your software as well.
Which Platform Has a Bigger Market Share?
At the very beginning of this article, we indicated that Android is the undisputed leader in the mobile software market, with almost 71% market share. However, it is worth noting that the ratio of market shares between platforms may vary depending on the business niche for which the application is created. Moreover, there is rather old research that owners of iOS devices are more willing to download paid applications, while owners of Android devices prefer free software. As a result, this factor can determine your monetization opportunities for your app, too.
Which Platform Has More Customization Options?
In terms of customization options, Android gives developers more flexibility due to the open nature of the platform. Thus, they get more space for creativity, which allows them to implement non-trivial designs and functionality. In turn, the iOS platform is a closed ecosystem with its own strict compliance rules. This concept is aimed at maintaining uniformity of user interfaces, so it will not be possible to create something too non-standard on its basis.
Android vs. iOS App Development: Which One to Choose
Ultimately, we cannot say that development for any one of the platforms, be it iOS or Android, is more profitable. Everything depends on the niche for which the software solution is being implemented, its localization, and many other factors that determine the size of the target audience.
Additionally, it is important to be aware of app store fees for paid software and software with in-app purchases. In particular, iOS paid apps, in-app purchases of digital goods or services, and/or linking out to purchase digital goods and services on your website are subject to a 17% fee (or 10% If you're enrolled in the App Store Small Business Program/the Apple Video Partner Program/News Partner Program or renew a qualifying auto-renewal subscription beyond one year); also, if you use App Store payment processing and related commerce services for in-app purchases, you will be charged a 3% fee. As for Google Play, here, the fee is 15% on the first $1 million in annual revenue (or 30% on annual revenue exceeding $1 million), 15% on products with an auto-renewing subscription (regardless of annual revenue size), and 15% or less for developers who qualify for the Play Media Experience Program.
By the way, if you find that the ratio of potential users for each platform is approximately 1:1, you can consider the cross-platform app development option, which involves creating a single code base for iOS and Android platforms. In this case, you can save about 30% of the budget compared to developing two native applications, and also bring the launch date of your mobile solution closer. The only thing is that, like any other type of software development, this one also has some restrictions.
Regardless of whether you are considering cross-platform or native mobile app development, you can always choose us as a reliable service provider of custom mobile solutions. We will implement your business idea with the minimum possible budget without compromising its quality and select the best approaches and tech stack to ensure its competitiveness and profitability over the long term.


According to data from the Precedence Research resource, the worldwide SaaS market is estimated at USD 358.33 bln in 2024 and is expected to grow up to USD 1,251.35 bln by 2034 at a CAGR of 13.3%. Such demand is due to the ease of deployment of such solutions (instead of local installation, access to them is possible from any device with a purchased license where there is an Internet connection), as well as often extensive customization options. If you would like to launch your own SaaS solution, but are not yet sure about the final list of features, you should consider the SaaS MVP development option.
What Is MVP in SaaS?
A minimum viable product (MVP) in the context of SaaS development is a version of a product where only the key functionality is implemented – that is, the one that determines the value of a specific SaaS solution for the end user. The goal of a SaaS MVP is to reduce development time by cutting down on secondary functionality, and to obtain user feedback to determine the course of implementation of a full-fledged SaaS version.
SaaS MVP Development Benefits
What are the benefits of SaaS MVP development? Let’s find them out right now.
Ability to competently plan a budget and attract investments
Compared to implementing a full-fledged SaaS solution, MVP development is cheaper, since its task is to allow the target audience to test its key functionality in practice, without any excesses in the set of features and user experience (UX) design. This simplifies budget planning, too, as it does not require colossal expenses from the project owners from the very beginning. Also, thanks to this approach to development, its speed increases. Therefore, the working product can be presented to potential investors a few months from the start of work, and it will not just be a business plan in the form of a presentation, but a functioning software solution that can be applied to solve specific tasks. Usually, negotiations regarding further investment in such a project with this strong attribute (an MVP) are successful.
High productivity of the development team
Since an MVP has a limited number of features, your team will be freed from optimizing user interface. Therefore, work on the MVP will proceed faster. In addition, when developing such a software version, your team may gain valuable insights that were initially overlooked – they can also be implemented over time. Finally, when the solution’s functionality is limited, it is easier for developers to identify possible areas for improvement and, thus, address them in further development cycles associated with the launch of a full-fledged SaaS version.
Reduced time to market
An MVP approach allows you to release your solution first. Indeed, given the rapid development of the global SaaS market, this would be a wise move. A couple of months delay needed for implementing a full feature set could cost you the fact that your product's analog will appear and win the audience's favor first. At the same time, by launching your product as early as possible, you will also be able to start refining it earlier, too, ultimately receiving a SaaS platform with a lot of functions and advanced user experience after 9-12 months from the start of work on the project.
Common Challenges of Building a SaaS MVP
Along with all the benefits, it is also worth considering the possible challenges associated with SaaS MVP development.
Impossibility of applying the MVP concept to absolutely all products
It is worth starting with the fact that MVP development is not a universal approach, and not all products allow for feature prioritization. In particular, this applies to the ones in which all functions are interconnected, and it is not possible to single out the most priority ones among them.
Breaks in development cycles
It is important to understand that the release of the MVP in its first version is not always followed by the development of a full-fledged product. Sometimes, the team has to implement one or two more solutions with limited functionality before its participants come to a full understanding of the concept of the SaaS solution. Since the collected feedback may relate to non-overlapping functions of the product, the preferences and dissatisfaction of real users may not be fully covered in the full-fledged product.
The need to adopt new approaches to software development
Quite often, the development of MVP is accompanied by the introduction of radically new practices, such as Agile development and DevOps. In the long term, iterative development and other methods can increase the team's productivity by about a third, but the adoption and training can also take a lot of time for the team.
Possible issues with the program code stability
Typically, MVP development of a cloud-based solution implies speeding up each development stage (in particular, the one related to testing the program code and its optimization). In this regard, it often happens that teams pay insufficient attention to the code stability, and the MVP solution itself becomes susceptible to hacker attacks. That is why, regardless of the chosen development approach and methodology, developers are still better off adhering to generally accepted standards for user data security and using proven authentication/authorization methods, reliable encryption protocols, access rights delimitation, etc.
Difficulty of scaling
Even though the MVP is initially hosted in the cloud, its computing power may not be enough if the product becomes really popular. In this regard, when choosing a cloud provider to ensure a scalable architecture, it makes sense to initially focus on options that allow automatic scaling as the workload on the software changes. Today, such type of service is provided by AWS, Microsoft Azure, and some other cloud vendors.
Problems with long-term budget planning
Lack of a clear understanding from the very beginning of what set of functions will be present in the final solution can provoke difficulties with budget planning, which, in turn, carries certain risks for investors. Therefore, it is important for you as a product owner to discuss with them all possible risks and prospects of your MVP launch strategy at the early stages of your interaction.
How to Build a SaaS MVP
So, how to build SaaS product – you may ask. Therefore, let’s consider the main steps you have to perform to develop an MVP.
Defining the target audience
First, you will need to understand who the target audience of your SaaS solution is and what they expect to get from it. In fact, you will have to collect demographic and behavioral data about your product users to determine the most important functionality for the MVP and provide them with the most comfortable ways to interact with it.
Market research
To give your SaaS solution a unique selling proposition (i.e., to make it stand out from the competition in some way), you will need to conduct preliminary research that will determine both market trends in general and help identify the strengths and weaknesses of your competitors.
Identifying core functionality
Now, you have everything ready to determine the functionality that is the highest priority for your SaaS solution. Usually, this is the functionality that allows you to solve one or two key tasks assigned to your product (that is, without it, it will lose its value for the end user).
Choosing a business model
At this stage, you need to come up with ways to monetize your product. Note that in the context of SaaS, this is most often the purchase of either a license for a certain period of use or access to advanced functionality.
Building a roadmap
Now, you can create a step-by-step plan for implementing your solution, from MVP to launching and supporting a full-fledged SaaS product. Note that this is necessary not only for presenting the prospects of your project to investors and stakeholders, but also for the technical team to make them understand in which direction to move.
Creating an MVP
At this stage, your technical team can begin to build MVP, i.e., implement its user interface, server requests, database requests, alpha testing, etc.
Deploying an MVP and collecting user feedback
Once your team is confident that the MVP meets the previously defined specifications and everything works as intended, you can deploy it to the production environment and begin beta testing – that is, testing it on real users to gather feedback on possible improvements. After that, you will have to prioritize the aspects highlighted by users and plan to implement them in subsequent development cycles.
How to Accelerate SaaS MVP Development
Finally, let’s consider a number of best practices that will help you speed up the SaaS MVP development process:
- Use Backend as a Service (BaaS) and low-code solutions to reduce the amount of work for your backend and frontend specialists, respectively;
- Choose a time-tested technology stack that all members of your development team are familiar with;
- Delegate individual tasks within your project or the entire project to an outsourcing service provider to eliminate the need to urgently search for talent with the necessary skills;
- Establish processes for collecting feedback from users from the very beginning of work on your project.
SaaS MVP Development with Darly Solutions
Would you like to build an MVP as a Service solution and are looking for a seasoned team of developers who will bring your business idea to life? In this case, feel free to contact us. MVP as a Service is one of the key areas of our activity, which you can see for yourself by requesting our portfolio. You can also entrust us with individual tasks within your project, such as QA testing or, for example, UI/UX design. Whatever the list of our services you choose, rest assured that you will be satisfied with the results of our cooperation!


The mobile apps market is rapidly growing. According to Grand View Research, the global mobile app market was evaluated at approximately USD 253 billion in 2023 and is going to grow with a 14.3% CAGR by 2030. That’s why the need for qualified mobile development specialists is so relevant today.
At the same time, one of the key features of a competent specialist is knowledge of the software development life cycle (SDLC) and which of the existing models is best to use in a specific project. The following article will overview the most popular SDLC models and explain where to apply them for the best results.
What is the Software Development Life Cycle (SDLC)?
The software development lifecycle is a methodology that guides the development team during the app creation process. Each of the development life cycle phases has its aims, timeframes, and challenges. Yet, a systemized approach toward software development ensures that the final product is of the highest quality.
In comparison, there are other approaches to software development. For example, development teams can choose from the following options:
- Application lifecycle management. It has a broader scope outside of the actual development process. It can include several SLDC development life cycle stages inside.
- Software testing lifecycle. This method emphasizes debugging and elimination of possible errors in the product.
- Product development lifecycle. This strategy includes market and product promotion after its development is complete.
What Is the Purpose of the Software Development Life Cycle (SDLC)?
The SDLC’s clear division into development cycle stages ensures that software is developed in a controlled environment. The systematic approach helps to avoid such challenges as:
- Budget breaches.
- Project overruns and crunches
- Failure to meet the requirements
- Expired deadlines
Creative freedom is important during the software development process. Yet, the SDLC approach ensures that all the creativity and revolutionary solutions are channeled constructively.
While following the life cycle of software development, each team member knows what task they should do and its deadline.
What are the 7 Phases of SDLC?
There are seven common SDLC phases:
- Requirements analysis
- Planning
- Design
- Development
- Testing
- Deployment
- Maintenance
Let’s consider them in more detail.
Requirements Analysis
It is the initial stage at which the developer's team evaluates the required features for the app. It defines how long the app will be in development, the budget’s size, and the deadlines.
This step answers such questions as:
- What is the objective of the app?
- Is it an upgrade or a brand-new software?
- What are the expected results?
Planning
The project can be planned after its goals and desired results are established. Planning in SDLC defines the technological stack and project roles. The project roadmap is also developed during the planning phase of SDLC.
Design
The software blueprint is created during the design stage. Ideas turn into features, architecture, and UI/UX design. Designing also includes consideration of the software's platforms and security as a part of SDLC processes.
Design can undergo several iterations before reaching its final look. During this phase, teams usually create a software prototype to see how all the features work together. This phase concludes with design document specification — a text description of the app’s functionality to share with stakeholders and within the team.
Development
Development is the long-lasting of the SDLC steps. During this stage, the team implements planned features and functionality into actual software. Tools for progress tracking and version control, such as Git, are common in the software development stage.
Testing
Testing comes after the implementation phase in SDLC. It is a rigorous process during which all software elements are evaluated. Testing can include:
- Performance testing
- Security testing
- Integration testing
- Alpha and beta testing, and so on
The result of the testing and debugging software development cycle phases should be a product meets its specifications and is ready for the commercial environment.
Deployment
Usually, the apps undergo testing and development in a secluded, special environment. Deployment implies transferring the software to the commercial space. The deployment phase includes final testing of the working product and gathering feedback from a limited audience.
The product is ready for full-fledged commercial use when the software development stages are over.
Maintenance
Maintenance is the final stage of the SDLC cycle. It includes software updates, security, and performance optimization. An upgrade or upscale of the software may be required in the future. In this case, the SDLC begins from the first stage, and the major update undergoes all the steps mentioned.
Most Common SDLC Models
The SDLC standards are common across the industry and development teams. However, there are different SDLC models. Each model serves its own purpose and offers a different order in which the different phases are performed.

SDLC Agile Model
The Agile SDLC model is the hallmark of modern industry. This model implies dividing the bigger tasks into smaller chunks and working on their implementation. The Agile method emphasizes communication between cross-functional teams and stakeholders.
Agile also implies frequent feedback gathering and analysis. Rigorous quality control is also an integral part of the Agile model.
SDLC Big Bang Model
The Big Bang model is an almost informal approach to the SDLC cycle. It ignores any planning or assessment and jumps straight into the coding. Such an approach is more risky than others. However, the model works best if delivery time is critical.
The Big Bang model can work for you if you wish to experiment or test waters in new markets.
SDLC DevOps Model
DevOps is a combination of development (Dev) and operations (Ops) teams to streamline the delivery of software products. The combined practices require service providers of highly skilled specialists. The main DevOps principles are continuous integration and delivery at the enterprise software development level. These methods help automate the process and streamline management tasks.
The DevOps model can strain the budget. However, the result is worth the cost. The DevOps SDLC cycle ensures that the product is in a deployable state and can be swiftly modified.
SDLC Iterative Model
An Iterative model is another representative SDLC cycle. Unlike the Agile model, iterative SDLC does not require continuous customer involvement. Besides, the iterative model has a more defined structure.
The Iterative model implies iterating the software and making changes between the cycles. Such an approach works well for expanded teams and allows the desired results to be achieved without failing deadlines or breaching the budget.
SDLC Lean Model
The Lean model is one of the oldest SDLC cycles that has persisted until today. It aims to achieve maximum efficiency in resource management. Unlike Agile, it focuses on the highest possible quality instead of close and consistent communication with the client.
It also takes a broader than Iterative model approach and improves the overall development process rather than the product itself. Lean is more philosophy than a precise model. As an SDLC model, Lean will ensure the quality of the product and client satisfaction before everything else.
SDLC Spiral Model
The Spiral model is a combination of Iterative and Waterfall models (this one will be discussed below), taking the best features from both approaches. The model consists of spirals, and each spiral has the following steps:
- Planning
- Risk analysis
- Development
- Testing
Such an approach allows risk mitigation at the early stage of the project. While being time-consuming, the Spiral model can be a fail-proof net for your project.
SDLC Waterfall Model
If you are looking for something straightforward and easy to manage – the Waterfall model is your choice. It takes the SDLC structure at face value and follows each step consecutively. The Waterfall model has its risks. It is rigid, and if changes or feedback appear in later stages, it will be hard to implement them. At the same time, the Waterfall model struggles with scalability.
On the other hand, it can spare the headache of complex management and task delegation.
Conclusion
Software development is a complex process that requires structure and precision. The Software Development Lifecycle provides such a structure. In seven steps, a software development team can clearly see goals and meet the client’s requirements.
Various SDLC models fit different needs and project scopes, and we know how to work with all of them. If you need specialists for custom software solutions, we are ready to answer your call and create a high-quality product. Contact us to discuss your project in detail.


According to Statista, in 2020, there were 6.9 billion mobile users. The number will increase to approximately 7.5 billion in 2025. Businessmen, students, housekeepers, gamers, readers, and sportsmen – everyone will need an app to satisfy their needs, and the demand for mobile app developers is high accordingly.
Yet, not every app finds its faithful audience. Only the best and highest-quality applications win the competition. Such applications require proficient mobile app development specialists. So, which skills distinguish a professional mobile app developer from a novice in 2024?
Stick to the article and learn what relevant skills you should look for in a full stack mobile app developer.
Top Hard Skills for Mobile App Developers
Hard app developer skills are the backbone of any mobile app development process. They define professional competence and allow developers to bring ideas into working digital solutions.
The most common hard skills for a mobile app developer are:
- Proficiency in programming languages for mobile app development (Java, C++, or Kotlin for Android, Swift or Objective-C for iOS, or JavaScript, Dart, or some other that is used for cross-platform development);
- Frontend development skills (SDKs and frameworks knowledge, understanding platform requirements, ensuring compatibility with different devices and OS versions, etc.);
- Backend development skills (database management, performance optimization, ensuring security measures, experience with backend frameworks, etc.);
- User interface (UI) design (including knowing the specifics of Google Material Design and iOS Human Interface Guidelines);
- Knowledge of RESTful APIs;
- Performance optimization and memory management skills;
- Experience in working with version control systems;
- Knowledge of app stores’ and other software development standards (like GDPR, HIPAA, etc.).
Top Soft Skills for Mobile App Developers
Hard skills are an essential but not the only necessary part of a developer’s competence. Soft application developer skills also play a critical role in CVs as they refer to knowledge and proficiencies related to communication and analytics. Also, they help organize the working process, solve problems, and build communication. When two developers with the same background in hard skills compete with each other, the one with stronger soft skills wins.
Top soft skills for a modern mobile app developer include the following:
- Problem-solving
- Team collaboration
- Project management
- Communication skills
- Attention to detail
- Creativity in app design
Most Important Mobile Developer Skills in 2024
Trends constantly change, but the demand for high-quality mobile applications remains the same. This block will explore the critical mobile app developer skills you should look for in a mobile app developer.
UI and UX Design
It's all about creating what users see on their screen and how they will interact with it. Usually, specialists follow generally accepted design rules (for example, Nielsen Norman's Heuristics), taking into account the requirements of the specific mobile platform for which development is being carried out. At the same time, native development tools provided by Android and iOS in particular, Jetpack Compose and SwiftUI significantly simplify this task, so experience working with them in the list of the most-wanted mobile developer skills will be highly preferable.
Frontend Development Skills
If we are talking about native development, the modern software engineer must have good programming skills in Swift for iOS development and Kotlin for Android development. However, some projects may also require knowledge of Objective-C, C++, or Java (for example, those that were developed a long time ago and need support), JavaScript or Dart (for cross-platform projects), or some other languages. Accordingly, the developer must have the necessary experience in frameworks for front-end mobile development, such as React Native, Flutter, Xamarin, SwiftUI, XCode, Android Studio, Native Development Kit, etc.
Backend Development Skills
The visual part of an app ensures the user’s engagement and experience with the app. The backend component is where the magic happens. A proficient back-end developer should know how to implement desired logic and manage the app’s inner data efficiently. A list of programming languages expands to Java, C#, Ruby, and Python, which are some of the most popular for backend development. Besides, a good backend developer should know how to work with mobile databases via SQLite, PostgreSQL, or MongoDB. Backend development also includes knowledge of API integration, which streamlines data exchange between an app's frontend and backend components.
User Security
Data safety and user authentication deserve additional attention. Knowledge of safe coding principles and best practices (i.e., using data encryption protocols, following the OWASP standard, and so on) is a marker of a skilled mobile app developer. Mobile developers must also have skills in conducting static application security testing (SAST) and dynamic application security testing (DAST).
Knowledge of Mobile Platform Guidelines
Due to the influx of applications to app stores, moderation has become stricter. Knowledge of the marketplace’s guidelines increases the chances of an app’s success. Actually, that’s why the list of iOS developer skills should include the knowledge of Human Interface Guidelines. He or she also should be familiar with Material Design guidelines for Android development. Knowledge of the review process should also be part of the developer’s competence.
Mobile App Developer Skills by Experience Level
The job market of mobile developers is versatile and can offer different levels of qualification. That’s why, if you are looking for a mobile app developer, you should also take into account a potential developer's performance.
Junior-Level Mobile Developers
Junior mobile app programmers are prospective specialists with no more than 2 years of experience. At this level, a specialist should be familiar with:
- UI/UX design principles
- Programming languages for mobile app development
- Mobile app development frameworks
- Version control systems and databases
It is important to understand that hiring a junior does not mean that you will have to supervise the entire project to get a good result in the end. These specialists can easily be entrusted with simple tasks (which will save you from overpaying for specialists with higher qualifications), up to 50% scope of work.
Middle-Level Developers
These are specialists with 3-5 years of experience. A middle-level developer's main focus is learning how to scale an application and ensure its security and operational stability. The following mobile application developer skills needed to reach mid-level app development proficiency are essential:
- Specifics of integration with third-party services and APIs
- Cross-platform adaptation
- Knowledge of the best security practices
- Asynchronous and multithreading programming
- Knowledge of popular architectural patterns like MVVM, MVC, MVP, etc
Vital Skills for Senior-Level Developers
Senior developers usually have 5+ years of experience and lead development teams. They take on the most challenging and responsible tasks within a project and know how to solve them in the simplest way. Also, they can be experts in certain technologies, like AI, IoT, augmented reality, etc. Actually, here's why the knowledge of blockchain in mobile apps can be required for them.
Senior developers help the rest of the team with ongoing tasks and can take on some managerial duties. Therefore, the CV of a senior mobile app developer would benefit from the following soft skills:
- Leadership
- Interpersonal communication
- Teamwork
- Time management
Most Underrated Skills for Mobile App Developers
Technical prowess is paramount for cross-platform app development. Still, certain skills are often overlooked when hiring a mobile development specialist.
Critical Thinking
Critical thinking is a cornerstone of every other mobile developer skill. It lies in the base of problem-solving, code optimization, and debugging. A critical approach is the ability to remain flexible and tackle challenges from unexpected angles.
It is hard to measure critical thinking in hard numbers. Yet, even a junior developer with strong critical thinking and analytical skills can greatly benefit a team.
Creativity
Creativity is an elusive but vital skill for a mobile developer. Successful applications become popular not only because of flawless technical execution. They innovate and solve users’ needs like nothing else. From AI in mobile apps to IoT integration, there are numerous ways in which new technological advancements can be used in mobile app development.
There are numerous tasks that mobile apps can solve and help people with their everyday lives. A mobile developer's ability to be creative, innovate, and find what can be optimized is valuable at any professional level.
Learning and Adaptability
Constant technological advancement requires professional developers to update their skills. They should familiarize themselves with new technologies. Even senior developers have to keep up with the market evolution.
If a developer has an open mind and is ready to learn new methods and software, they will be a valuable asset to your project.
Conclusion
A professional mobile developer combines several important skills. He or she knows both the backend and frontend aspects of mobile app development. They also know the programming languages and tools to implement app ideas in the most cost- and time-efficient way. Most importantly, a mobile app developer keeps an open mind. They think creatively and approach problems from unusual angles. Darly Solutions is ready to assist with your project if you need such professionals. Contact our dedicated team to learn more details.

Connect with us
.webp)
We are a tech partner that delivers ingenious digital solutions, engineering and vertical services for industry leaders powered by vetted talents.
