Most common AI technologies used in digital therapeutics
Digital therapeutics (DTx) platforms now integrate AI not as experimental add-ons to engines powering entire clinical functionalities. Artificial intelligence in healthcare drives personalization. It automates intervention delivery and generates evidence-based outcomes.
Yet, understanding which AI technologies deliver measurable impact and which remain overhyped is critical to platform strategy and regulatory pathways.
This article breaks down the most deployed AI approaches in DTx and maps them to specific clinical use cases. It also provides a basic implementation roadmap that companies can build their strategies upon.
Why AI Is Now Core to DTx
The UK’s National Institute for Health and Care Excellence (NICE) states that AI methods may offer superior approaches to evidence generation for health technologies. AI in digital therapeutics can efficiently process and analyze large datasets. It reveals patterns and relationships that may not be readily apparent to human analysts.
The European Commission also sees AI as a transforming force in medicine. It is expected to enhance equity, improve care, and ensure that new technologies, treatments, and medicines benefit society at large. Hence, over the past few years, the EU has been developing legislation for the use of AI in healthcare.
There is a whole range of features that make digital therapeutics suitable for AI integration:
- Personalization. AI algorithms analyze patient data to deliver customized therapeutic interventions based on individual response patterns.
- Real-time monitoring. AI in patient monitoring, with continuous tracking of patient metrics, enables timely interventions and risk prevention.
- Predictive analytics. AI models forecast disease progression, relapse risk, and treatment outcomes to implement proactive care strategies.
- Scalability. AI scalability in health tech makes evidence-based care accessible beyond traditional healthcare capacity constraints.
Artificial intelligence is expected to play an ever-increasing role in next-generation DTx solutions as care models move towards prevention. In 2024, AI-focused companies already captured 42% of digital health funding and 31% of deals. Both are record highs. As for the consumers, 55% use AI in prevention-related decision-making. The share among 18–28-year-olds is above 80%.
AI integration could further differentiate DTx from other forms of therapeutics. Providers can achieve this by enabling a more personalized form of care that actively adapts to patients’ individual clinical needs, goals, and lifestyles. It all makes AI a differentiator that businesses can use to build up an advantage and create future-ready solutions.
Understanding Digital Therapeutics and Where AI Fits In
DTx products deliver evidence-based therapeutic interventions via innovative software. Unlike wellness apps that have been around for a while, DTx must demonstrate clinical efficacy through randomized controlled trials and meet regulatory standards.
Hence, the role of AI in this context is somewhat more complex. Technologies deployed for digital therapeutics AI integration fall under three functional categories based on their role in the therapeutic value chain:
- Core AI engines.
- Emerging generative and multimodal systems.
- Supporting the AI ecosystem.
Let’s take a closer look at each.
Top AI Technologies Used in DTx
Each of the abovementioned layers serves distinct roles in the DTx value chain. Understanding this taxonomy enables teams to allocate development resources effectively, sequence technology adoption appropriately, and address the relevant ethical challenges associated with AI in healthcare.
Core AI Engines
Core AI engines form the computational backbone of the system. They process clinical data and drive therapeutic decision-making. This category includes predictive analytics in healthcare, time-series models, and reinforcement learning algorithms. All influence treatment pathways directly: by selecting intervention content, predicting clinical trajectories, and optimizing therapy timing.
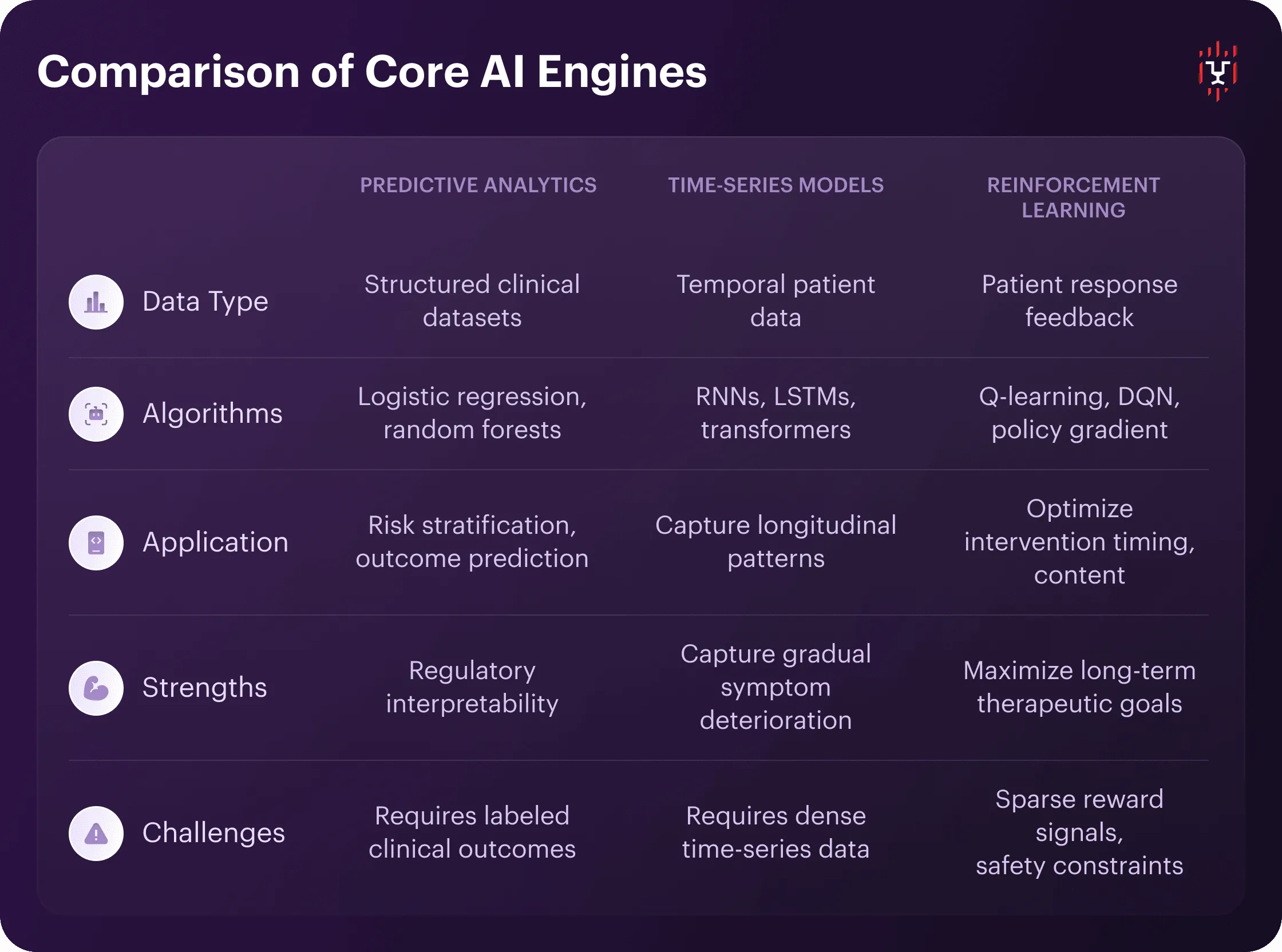
Predictive Analytics and Classical ML
Supervised learning models dominate DTx risk stratification and outcome prediction. These algorithms include logistic regression, random forests, and gradient boosting, among others. All are trained on structured clinical datasets.
Examples of such algorithms are XGBoost and LightGBM. They can classify patients (e.g., high/low relapse risk in substance use) or predict continuous outcomes (PHQ-9 score trajectories in depression management).
The strength of the classical machine learning in digital health lies in regulatory interpretability. Meeting the requirements of explainable AI in digital medicine is critical for adaptive algorithms. Implementation requires labeled clinical outcomes and ongoing validation as user populations shift.
Time-Series/Sequence Models
Recurrent neural networks (RNNs), long short-term memory networks (LSTMs), and transformer architectures process temporal patient data. It can include continuous glucose readings, daily mood/activity logs in mental health apps, sensor streams from wearables, and more. They capture longitudinal patterns that static feature sets miss, such as gradual symptom deterioration, cyclical behavior changes, and treatment response lag effects.
Sequence models require dense time-series data. It must be at least 30–90 days per patient, with daily or more frequent observations. In some cases, transformer models adapted from NLP can outperform LSTMs on irregular sampling patterns common in real-world DTx data.
Reinforcement Learning for Adaptive Interventions
RL algorithms — Q-learning, deep Q-networks (DQN), policy gradient methods — are the core of AI for personalized medicine. They learn from patient response feedback to optimize intervention timing, content selection, dosing, etc. Unlike supervised models, RL agents don’t predict outcomes. They actively experiment to discover which actions maximize long-term therapeutic goals, such as sustained abstinence and symptom remission.
RL implementation faces two DTx-specific challenges. One is sparse reward signals, with clinical outcomes occurring weeks or months after interventions. The other constraint is safety, meaning that exploration must not harm patients. Regulatory agencies expect rule-based boundaries that prevent RL agents from recommending contraindicated actions.
Emerging Generative and Multimodal Systems
Emerging generative and multimodal systems represent the current innovation frontier. They utilize large language models and sensor fusion to create more naturalistic interactions and capture richer clinical signals. Large language models (LLMs) power conversational interfaces for patient support and assessment. Computer vision and speech analysis extract digital biomarkers from non-traditional data streams.
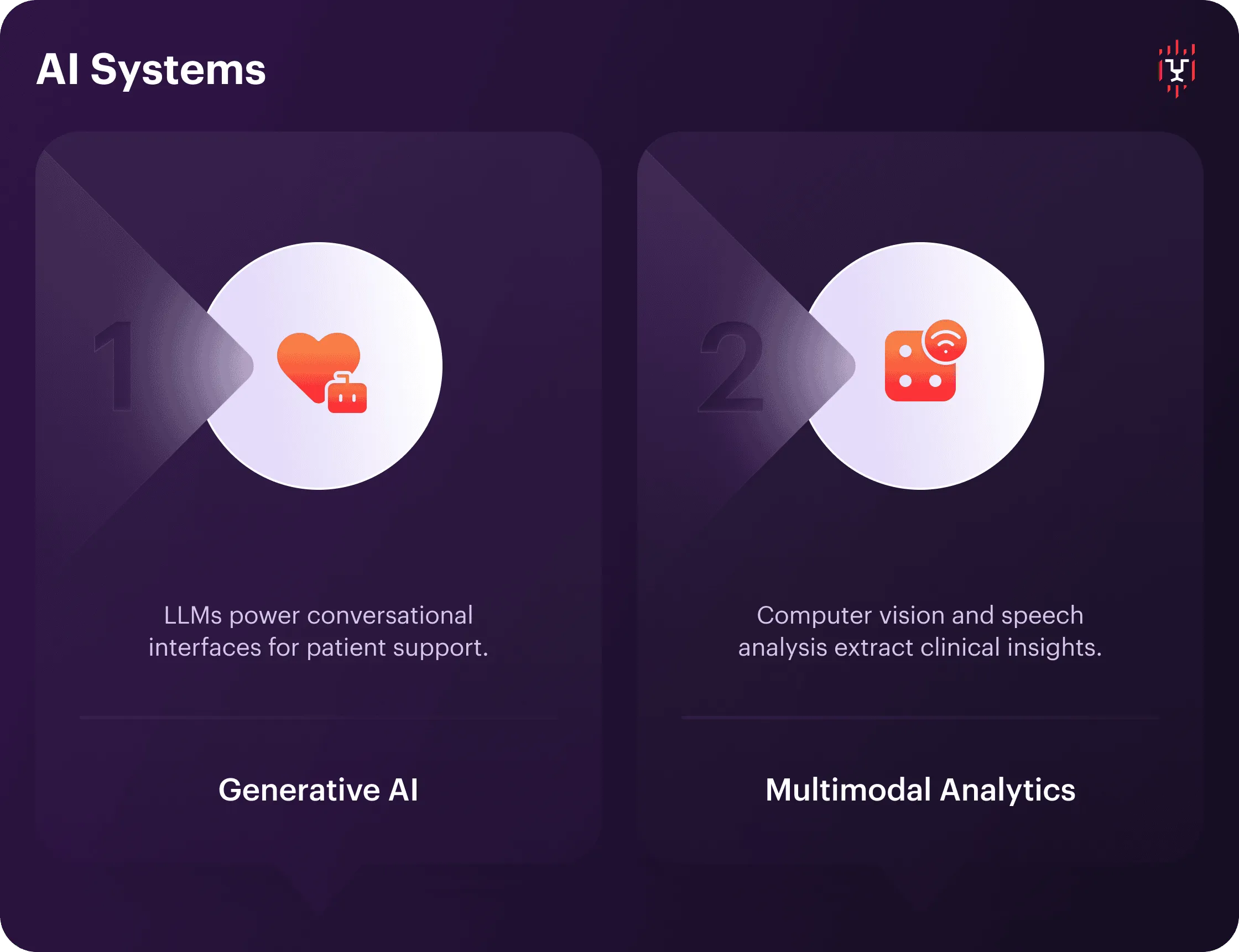
Generative AI and Assistants
LLMs such as GPT, Gemini, Claude, etc., power conversational interfaces that conduct intake assessments, deliver psychoeducation, and provide empathetic responses. They perform well in mental health and chronic disease DTx. Generative AI in healthcare moves beyond rigid chatbot decision trees to handle open-ended patient questions and provide contextually appropriate content.
Regulatory caution around LLMs centers on hallucination risks and unpredictable outputs. Practical implementations use retrieval-augmented generation (RAG) to ground LLM responses in validated clinical content libraries. It’s also critical to employ output filtering to block potentially harmful suggestions.
Multimodal Analytics and Digital Biomarkers
Computer vision and speech analysis algorithms extract clinical insights from non-traditional data streams. Some examples of the latter are facial expression analysis for depression monitoring, voice biomarkers for Parkinson’s progression, and gait pattern recognition from smartphone accelerometers.
These digital biomarkers enable passive symptom tracking without requiring active patient reporting. They reduce burden while capturing data that clinicians cannot observe in brief office visits. However, multimodal approaches require significant validation. Each digital biomarker needs independent evidence linking the measured signal to clinical outcomes.
Supporting AI Ecosystem
A supporting AI ecosystem does not directly implement therapeutic algorithms. It provides the data infrastructure and user touchpoints that enable DTx AI to function in real-world settings. This layer handles data collection, quality assurance, and integration. Mobile app frameworks, wearables, and IoMT devices make AI usable and feed these models.
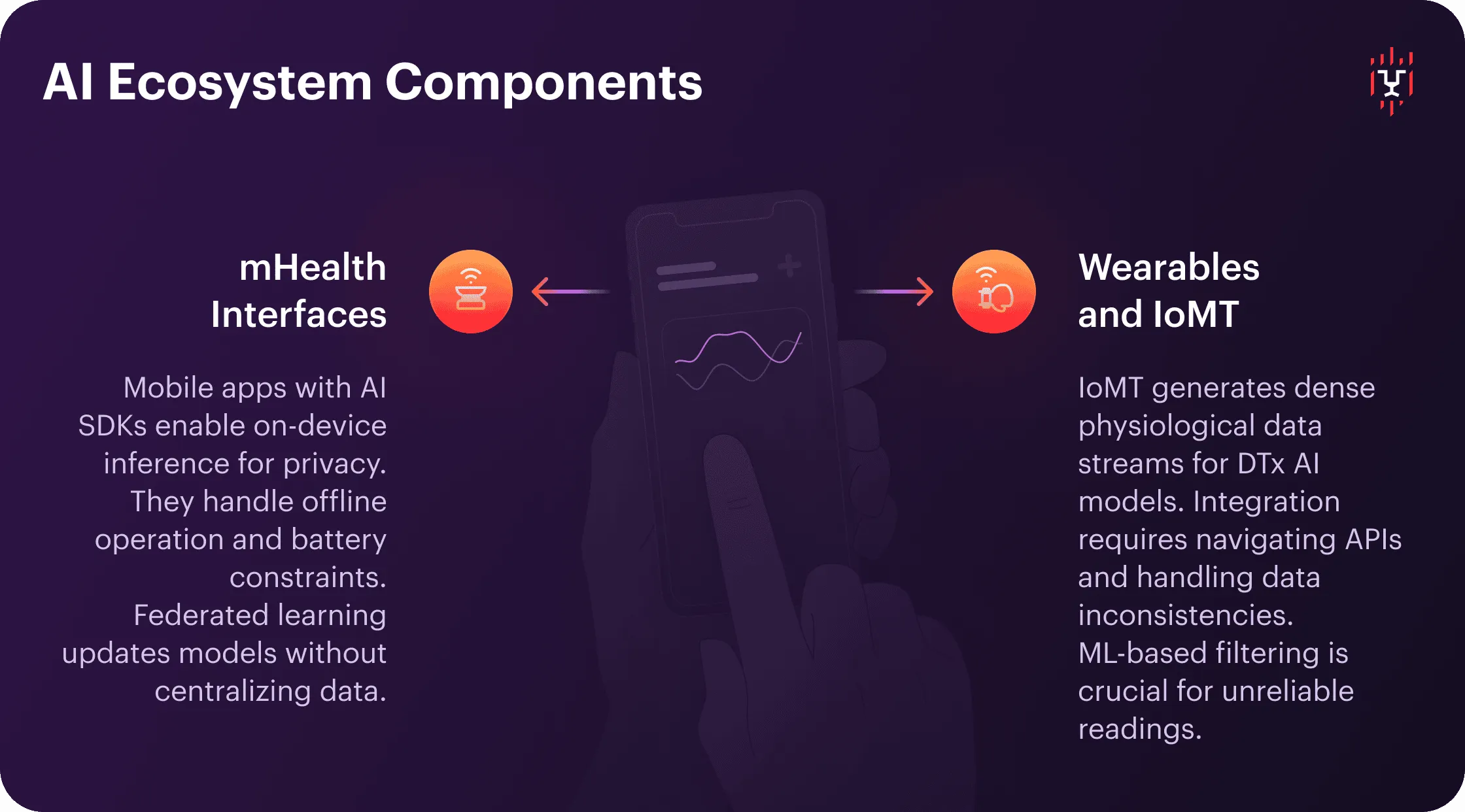
mHealth Interfaces
Mobile application frameworks with embedded AI/ML software development kit (SDK) enable on-device inference for privacy-sensitive DTx features. The latter includes features such as real-time emotion detection from journal entries and immediate AI-driven behavioral interventions based on sensor data.
mHealth infrastructure must handle offline operation (patients lose connectivity) and battery constraints (continuous sensor monitoring drains power). Federated learning approaches now allow model updates across distributed mobile devices without centralizing patient data, addressing both privacy and scarcity challenges.
Wearables and IoMT
The Internet of Medical Things (IoMT) generates dense physiological data streams that feed DTx AI models. Their integration requires navigating vendor-specific APIs, handling data format inconsistencies, and running quality checks for sensor artifacts. Continuous glucose monitors, ECG patches, actigraphy bands, and similar devices can occasionally generate unreliable readings. ML-based filtering before clinical use is paramount.
The complexity of regulatory compliance for AI DTx apps increases when wearable data drives therapeutic actions. FDA distinguishes between general wellness devices and medical-grade sensors. DTx teams must document data lineage. It involves identifying the sensor readings that feed specific algorithms and enabling traceability for adverse event investigations.
Technology Selection Framework
“The DTx companies succeeding in 2026 aren’t those designing the most complex logic. They are deploying the right AI for their purpose and maturity stage. As proven from experience, AI differentiation comes from clear evidence and relevant strategy, not from following trend cycles.”
Daria Lymanska, CEO, Darly Solutions
High-Value Clinical Use Cases for AI in DTx
The real-world evidence for AI-based therapies is already evident in terms of both clinical and economic impact across various therapeutic categories. Below, we share several cases from areas of application where artificial intelligence makes a significant difference.
AI for Chronic Disease Management
AI-driven digital health solutions that generate real-time intervention recommendations are valuable for managing chronic diseases. Medical systems already integrate continuous glucose monitors, blood pressure cuffs, activity trackers, and similar devices. With AI, predictive models can analyze meal logs, medication timing, exercise patterns, biometric trends, and more to forecast crises and enable preemptive interventions.
In other words, doctors get AI to personalize self-care recommendations for patients who need them for their lifetime. By analyzing symptom tracking data, the applications identify areas for improvement and help each user better manage their condition. This optimizes both time and spending for patients and care providers.
NLP for Mental Health Apps
Depression, anxiety, and substance use disorder DTx deploy NLP models to analyze patient text inputs — journal entries, chat messages, etc. These recordings serve as symptom severity indicators and suicide risk markers. Sentiment analysis tracks mood trajectories across CBT session sequences, flagging patients whose PHQ-9 or GAD-7 proxy scores deteriorate despite treatment engagement.
Time-series models predict relapse risk in substance use. It is possible through the analysis of engagement drop-offs, self-reported craving patterns, geolocation data (proximity to high-risk locations), and wearable device-detected sleep disruptions. Integrating AI into contingency management protocols allows for building an adjustable reward system based on predicted relapse windows.
AI in Rehabilitation Technology
Post-stroke, orthopedic surgery, and neurological condition DTx use computer vision and sensor fusion. These applications make it easier for patients to monitor exercise adherence and movement quality during home-based rehabilitation — and they make rehabilitation safer. Smartphone cameras or depth sensors capture range-of-motion metrics, repetition counts, and compensatory movement patterns that indicate incorrect technique.
Long short-term memory (LSTM) models can predict adherence drop-off. They analyze exercise completion rates, report pain levels, and track session duration trends. AI defines the probability of program abandonment when detecting the engagement patterns associated with it. The system triggers retention interventions, such as therapist check-ins, exercise difficulty adjustments, motivational content, etc.
AI for Preventive Care
Diabetes prevention programs, hypertension screening, and cancer risk assessment in DTx use classical ML models to stratify populations and target high-risk individuals for intensive interventions. Computer vision in medical applications screens photos for skin cancer risk and diabetic retinopathy progression, directing high-risk cases to specialist evaluation.
These tools augment rather than replace a clinician’s diagnosis. AI serves as a triage mechanism to prioritize limited specialist capacity. Yet, it is another level of precision and speed in detecting severe conditions that clinicians acquire.
AI for Medication Adherence
Studies on non-adherence globally date back a few years, but each cites hundreds of billions in direct costs and thousands of deaths. DTx addresses this through multiple AI mechanisms. Computer vision confirms pill ingestion. AI chatbots in digital therapy send contextually optimized reminders. Predictive models identify adherence risk from refill patterns and self-report inconsistencies.
Current-generation adherence DTx focuses on behavioral interventions rather than invasive sensors. AI analyzes pharmacy claims, app engagement logs, patient-reported barriers, and other data to generate personalized adherence strategies. It can time medication doses and align them with daily routines, provide side effect management content, navigate through cost assistance, and more.
AI Integration Roadmap for DTx Startups
Deploying AI technologies in digital therapeutics requires a structured phasing. Companies are to balance technical stack, clinical validation requirements, regulatory expectations, and risk mitigation. The four-phase approach below reflects patterns that have proven to be efficient.
Phase 0: Use-Case Scoring
Always begin with AI model validation in medical devices. Prioritize AI opportunities using quantifiable criteria that align with organizational strategy and market readiness. Create a scoring matrix evaluating potential use cases across five dimensions:
- Clinical impact potential: measured by targeted outcome metrics like hospitalization reduction or symptom remission rates.
- Data availability and quality: volume of labeled examples, missing data rates, demographic coverage.
- Regulatory pathway clarity: precedent FDA clearances in similar indications.
- Payer reimbursement likelihood: existing CPT codes or coverage policies.
- Technical feasibility given current team capabilities.
This framework prevents the common pitfall of pursuing technically impressive AI applications that lack clear paths to clinical validation or revenue.
Phase 1: Pilot
Pilot deployments validate core technical assumptions and clinical utility with 50–200 users over 8–16 weeks under protocols approved by the institutional review board. Primary objectives include gathering real-world evidence for AI-based therapies and identifying data quality issues that require pipeline improvements. Teams can also collect user feedback on AI-driven recommendations from both patients and supervising clinicians.
Phase 2: Validation and Scale
Validation studies provide the clinical evidence that regulators and payers require for clearance and reimbursement decisions. Design depends on AI’s role in the therapeutic mechanism — whether it directly drives treatment decisions or serves a supportive role. Concurrent with clinical validation, engineering teams prepare for migrating from pilot infrastructure to production scale.
Phase 3: Continuous AI Optimization
AI model performance degrades over time — as patient populations shift, clinical practices evolve, and data distributions drift from training sets. Establish continuous learning pipelines that retrain models at least quarterly or triggered by drift detection thresholds. This ongoing optimization cycle transforms DTx from static software to ever-evolving health systems.
.webp)
Building AI-Powered DTx Platforms with Darly Solutions
Our company has almost ten years of experience working with digital platforms of various complexities for hospitals and clinics, diagnostic labs, and imaging centers. This includes developing AI-powered digital therapeutics applications from scratch and integrating innovative technologies into clients’ existing software.
For example, a user app for operating an AI-driven neuroscanning system allowed our client to use the power of the real-time central neural system (CNS) scanning and speed up data processing by 23%. In another case, reworking the interface for a real-time PCR system and integrating advanced AI-powered analytics improved error detection rates by 18% and user productivity by 32%.
Key Takeaways
AI applications in digital therapeutics have transitioned from experimental features to a foundational infrastructure.
Classical machine learning and time-series models now power risk stratification, outcome prediction, longitudinal monitoring, and many more functionalities. Generative and multimodal AI systems facilitate natural language interactions, thereby reducing patient burden. And it’s already “a must” rather than “nice-to-have.”
Yet, to design an innovative product, companies need to go through a long process of development, validation, compatibility testing, and continuous improvement. Transforming DTx from static software into learning health systems that boost efficiency requires niche expertise that our team possesses and is ready to provide.
If you're seeking proven AI expertise in healthcare, contact us and let’s transform your ideas into a high-performing digital platform.
FAQ
Classical machine learning models — XGBoost, random forests, logistic regression — deliver the highest measurable impact in current DTx deployments. Time-series models (LSTMs, transformers), reinforcement learning algorithms, and generative AI demonstrate efficiency when it comes to specific areas and functionalities. Digital twins in healthcare help optimize the algorithms and architecture without compromising system performance.
Data privacy in digital therapeutics, along with its availability and quality, presents the primary barrier. AI models require thousands of labeled patient outcomes for training, while DTx startups often have limited historical datasets. Regulatory uncertainty around adaptive algorithms increases development timelines, particularly for reinforcement learning systems. Additionally, the costs of clinical validation escalate with the complexity of AI.
AI enables true personalization at scale. It adjusts intervention content, timing, and intensity based on individual patient response patterns rather than applying one-size-fits-all protocols. AI also reduces clinician burden by automating routine monitoring and triage, allowing human oversight to focus on high-risk cases and complex decisions.
Patients with chronic conditions requiring continuous monitoring and frequent intervention adjustments gain the most clinical value. The same applies to high-risk populations. Meanwhile, AI in remote patient care helps stable patients avoid unnecessary clinical contact, optimizing resource allocation. Ultimately, all payers benefit.
Connect with us
.webp)
We are a tech partner that delivers ingenious digital solutions, engineering and vertical services for industry leaders powered by vetted talents.




.webp)
.webp)